The Affordable Care Act’s (ACA) Medicaid expansion has been a topic of debate in Tennessee since the U.S. Supreme Court made it optional in 2012. This post quickly introduces the issue and offers 6 lessons based on other states’ experiences with Medicaid expansion.
Key Takeaways
- TennCare expansion could provide significant federal funding to extend Medicaid eligibility to about 250,000 uninsured Tennesseans.
- Under current law, Tennessee would pay 10% of the long-term costs of expanding TennCare. Those costs could be difficult to predict because Medicaid is an entitlement.
- What can Tennesseans learn from other states’ experiences with Medicaid expansion? Data show:
- Low-income individuals’ access to care typically improves following Medicaid expansion.
- The costs of Medicaid expansion have been higher than many states expected.
- Medicaid expansion may increase access to addiction treatment for low-income individuals.
- Medicaid expansion may reduce (but not eliminate) the odds that a rural hospital will close.
- The costs and benefits of implementing Medicaid copays, behavioral incentives, and work requirements are not yet clear.
- Medicaid expansion may help reduce Obamacare premiums.
We’ll examine each of these points in greater detail below. First, a little background…
What Is Medicaid Expansion?
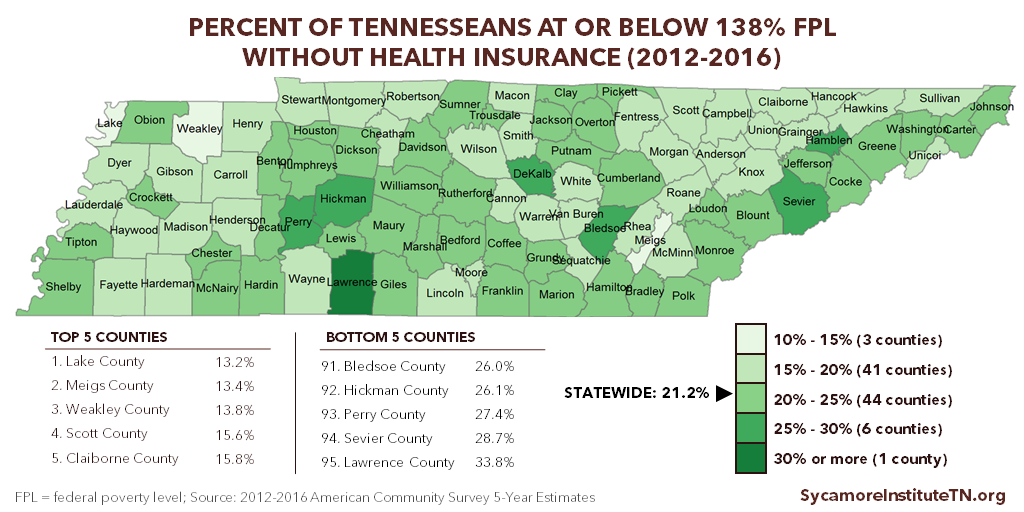
The ACA provides federal funding for states to expand Medicaid eligibility to all adults under 138% of poverty, which in 2018 amounts to $34,638 for a family of 4. (1) Expansion would make about 250,000 uninsured Tennesseans newly eligible for TennCare, Tennessee’s Medicaid program. (2) (3) As many as 163,000 of them do not currently qualify for TennCare or ACA subsidies for private insurance (i.e. “the coverage gap”). (2)
Tennessee has not expanded Medicaid eligibility under the ACA, so TennCare primarily serves populations required by federal law. These include low-income individuals in one of the following categories: children, pregnant women, parents or caregiver relatives, seniors, and individuals with disabilities. Childless adults without disabilities are largely ineligible for TennCare today.
Figure 1
Source: 2012-2016 American Community Survey 5-Year Estimates (7)
The Trade-Offs of Medicaid Expansion
Like all public policies, Medicaid expansion involves trade-offs. There are costs associated with expanding Medicaid and costs associated with not doing so. Here are a few of those trade-offs.
If Tennessee expands TennCare, the state would pay 10% of the long-term costs under current law. Proposals to date (discussed below) have used hospital assessments to pay these costs. TennCare costs can be difficult to predict because Medicaid is an entitlement, meaning anyone who is eligible can enroll. The state portion would be 6% in 2018, 7% in 2019, and 10% in 2020 and beyond, with the federal government paying the remainder. (4) The Robert Wood Johnson Foundation (RWJF) and the Urban Institute estimate Tennessee’s net share at $2.9—3.1 billion from 2018—2027, depending on enrollment. (5) There is also some risk that a future Congress could change the law to make states pay more of the cost. Tennessee pays about 35% of the costs of traditional TennCare enrollees.
If Tennessee does not expand TennCare, the state will continue to forgo significant federal funding that could help cover about 250,000 uninsured residents. Based on other states’ experience with Medicaid expansion, TennCare coverage has the potential to increase these individuals’ access to health care (see below). The same RWJF and Urban Institute study predicts net federal funding for TennCare expansion would reach $27.5—31.5 billion over the 10-year period. This money would generate new economic activity in the state and millions of dollars in sales tax revenues for state and local government, according to a study by the University of Tennessee. (6)
History of Tennessee’s Debate Over Medicaid Expansion
In 2015, the General Assembly rejected Governor Haslam’s proposal to expand TennCare, known as Insure Tennessee. Under the proposed 2-year pilot program, newly eligible individuals would have received a subsidy to purchase employer-sponsored coverage or been enrolled in a TennCare managed care plan. Tennessee’s share of the costs were predicted to be $92 million over FYs 2016-2017 and 2017-2018, financed by an assessment on hospitals. The federal share was predicted to be $2.2 billion over the same period. (8)
The 3-Star Healthy Task Force appointed by Speaker Harwell to explore other options outlined a 2-phased approach in 2016. Initially, TennCare expansion would have been limited to veterans and individuals with certain behavioral health diagnoses. If the state met certain goals and benchmarks, eligibility would then expand to every Tennessean with an income below 138% of poverty. (9) These efforts were put on hold following the 2016 presidential election.
The General Assembly and candidates for governor continue to debate whether or not Tennessee should expand Medicaid. The federal government’s recent approval of Medicaid work requirements in Kentucky, Indiana, and Arkansas adds a new wrinkle to that debate.
6 Lessons for Tennessee from Other States’ Experience with Medicaid Expansion
As the debate continues, what can Tennesseans learn from the experiences of other states that have (or have not) expanded Medicaid eligibility? Here’s a closer look at what the research shows.
1. Low-Income Individuals’ Access to Care Typically Improves Following Medicaid Expansion.
While coverage does not equate to care, most research indicates that low-income individuals’ access to care improves after Medicaid expansion, according to a Kaiser Family Foundation (KFF) review of 153 studies, reports, and white papers. (10) Many of the studies reviewed found that providers in expansion states increased capacity to meet the greater demand. The review did find 1 study showing an increase in reports of care being delayed due to appointment wait times. (11)
What limited data exist suggest that appointments for current TennCare enrollees may be more readily available than commonly believed. A 2017 survey of TennCare enrollees found that 71% waited 1 week or less for their most recent sick visit with a primary care physician, and a 2015 study found that most Tennessee physicians in 2013 accepted new patients covered by TennCare (76%) and private coverage (84%). (12) (13)
2. The Costs of Medicaid Expansion Have Been Higher than Many States Expected.
Nationwide, the average per-enrollee cost of the adult Medicaid expansion population was 49% higher than expected in 2015. (14) Adding to the cost overruns, more people have enrolled than many states anticipated. (15) Although overall per-enrollee costs for newly eligible adults fell in 2016 and were predicted to keep falling through 2018 (16), a more recent study of 9 expansion states found that per enrollee costs are likely to rise over time because older, less healthy individuals stay enrolled longer than younger, less healthy individuals. (17)
3. Medicaid Expansion May Increase Access to Addiction Treatment for Low-Income Individuals.
States that expanded Medicaid prior to the ACA saw an 18% drop in unmet need for addiction treatment services among low-income adults, according to a 2015 study. (18) In 2013, an estimated 64,000 low-income, uninsured Tennesseans had substance use disorders. (19) More recently, the Tennessee Department of Mental Health and Substance Abuse Services (TDMHSAS) estimated that about 23,000 Tennesseans who qualify for behavioral health safety net services have an opioid use disorder specifically. (20) Many of these individuals could become eligible for TennCare under expansion. Furthermore, opioid-related hospitalizations, overdoses, and cases of neonatal abstinence syndrome continue to rise in Tennessee.
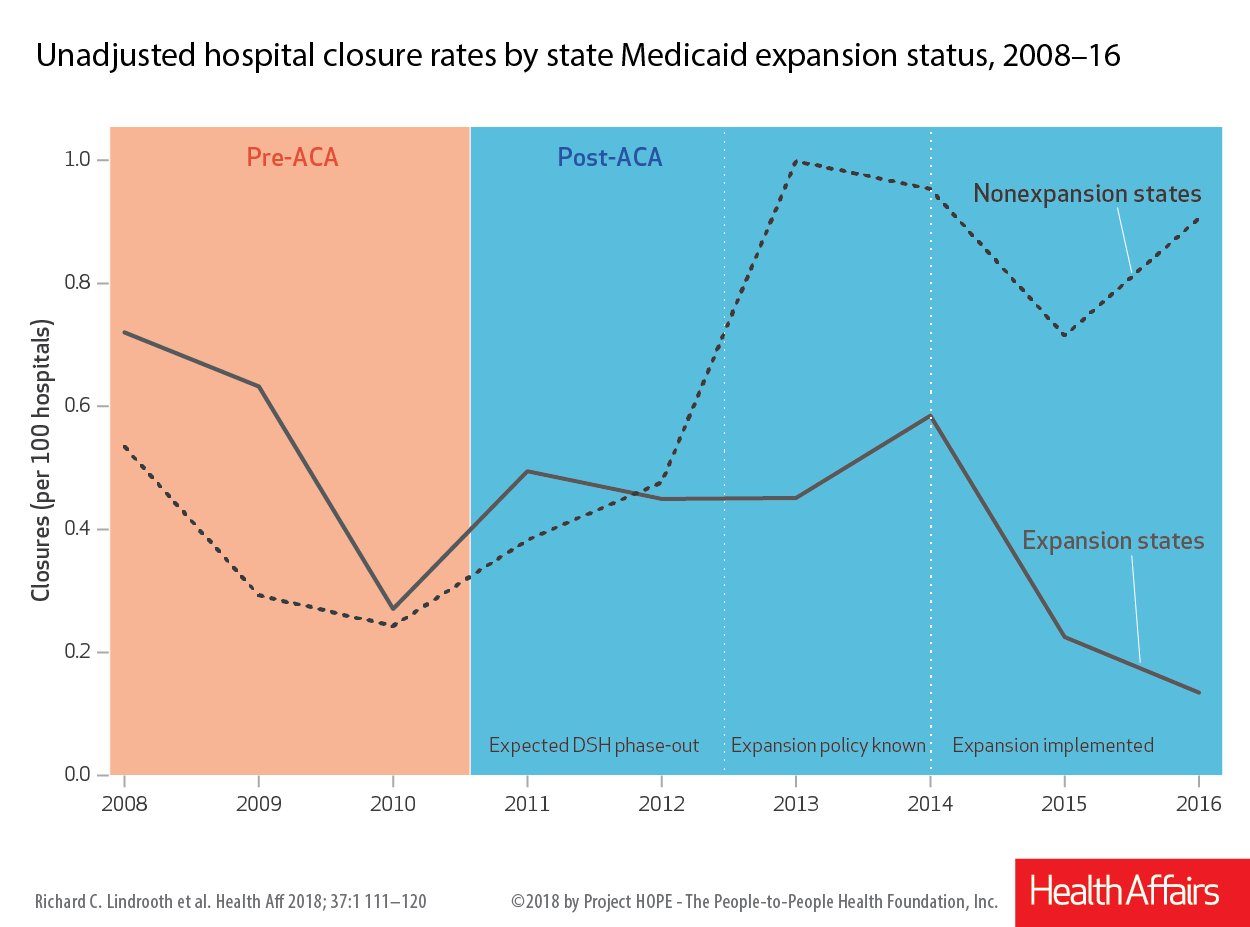
Figure 2
Source: Health Affairs (21)
4. Medicaid Expansion May Reduce (But Not Eliminate) the Odds that a Rural Hospital Will Close.
Rural hospitals in states that expanded Medicaid had stronger finances and were less likely to close than those in non-expansion states, according to a 2018 study. (Figure 2) (21) Many factors contribute to the national trend of rural hospital closures, including the industry’s shift away from inpatient care and rural populations often being older, sicker, lower-income, and shrinking compared to the rest of the country. By creating more “paying” customers for rural hospitals, Medicaid expansion may partially offset some of these financial pressures. Seven rural Tennessee hospitals have permanently closed since 2010, according to a list provided by the Tennessee Hospital Association.[i]
5. The Costs and Benefits of Implementing Medicaid Copays, Behavioral Incentives, and Work Requirements Are Not Yet Clear.
At least 7 states’ Medicaid expansion efforts include enrollee cost-sharing, healthy behavior incentives, or work requirements. (22) (23) Both the Insure Tennessee and 3-Star Healthy Task Force plans included similar enrollee responsibilities and incentives. (24) (9) It is too soon to evaluate the outcomes of these efforts to encourage healthier choices and use of higher-value health care. However, some recent studies suggest that their implementation has sometimes been expensive for states and confusing for enrollees. (25) (26) (27) (28) (29) Our 3-part series on Medicaid Work Requirements discusses some of the factors policymakers may want to weigh when considering any TennCare enrollee responsibilities.
6. Medicaid Expansion May Help Reduce Obamacare Premiums.
Health insurance premiums on the healthcare.gov Marketplace are lower in states that expanded Medicaid, according to 2 recent studies. (30) (31) In non-expansion states, the sickest of the potential expansion population often sign up for Marketplace coverage while the healthiest tend to go uninsured. This makes Marketplace risk pools more costly, which drives up premiums. Premiums in Tennessee’s Marketplace were some of the highest in the country in 2017.
Related Work by The Sycamore Institute
Medicaid Eligibility in Tennessee (August 30, 2017)
Understanding Medicaid and TennCare: Key Concepts and Context to Know (June 1, 2017)
Healthy Debate 2018: A Primer on Health and Budget Policy in Tennessee (January 5, 2018)
Medicaid Reform 101: More Than Just Block Grants – Part 4: Summary of Recent TennCare Proposals (January 26, 2017)
Medicaid Work Requirements in Tennessee (2017)
The Opioid Epidemic in Tennessee (August 2017)
Options for Stabilizing Tennessee’s Individual Market (July 20, 2017)
[i] Note: Over the last year, we have reported 3 different Tennessee rural hospital closure numbers. Our previous reports relied on a national rural hospital closure database maintained by the University of North Carolina. A June 2017 report cited 9 closures, and a January 2018 report cited 8, which reflected the reopening of 1 previously closed hospital in August 2017. Our current count relies on a list provided by the Tennessee Hospital Association, which includes 10 rural hospital closures since 2010. Of these, 1 is not technically designated as rural, and 2 are the same facility in Scott County, which closed and reopened twice. It is currently open and operating under a new name (Big South Fork Medical Center).
References
Click to Open/Close
- U.S. Department of Health and Human Services. U.S. Federal Poverty Guideline Use to Determine Financial Eligiblity for Certain Federal Programs. [Online] 2017. [Cited: January 1, 2018.] https://aspe.hhs.gov/poverty-guidelines.
- Garfield, Rachel and Damico, Anthony. The Coverage Gap: Uninsured Poor Adults in States that Do Not Expand Medicaid. The Kaiser Family Foundation. [Online] November 1, 2017. https://www.kff.org/uninsured/issue-brief/the-coverage-gap-uninsured-poor-adults-in-states-that-do-not-expand-medicaid/.
- Buettgens, Matthew and Kenney, Genevieve. What if More States Expanded Medicaid in 2017? Changes in Eligiblity, Enrollment, and the Uninsured. Robert Wood Johnson Foundation and Urban Institute. [Online] July 2016. https://www.urban.org/sites/default/files/publication/82786/2000866-What-if-More-States-Expanded-Medicaid-in-2017-Changes-in-Eligibility-Enrollment-and-the-Uninsured.pdf.
- Rudowitz, Robin. Understanding How States Access the ACA Enhanced Medicaid Match Rates. The Kaiser Family Foundation. [Online] September 29, 2014. https://www.kff.org/medicaid/issue-brief/understanding-how-states-access-the-aca-enhanced-medicaid-match-rates/.
- Dorn, Stan and Buettgens, Matthew. The Cost of Not Expanding Medicaid: An Updated Analysis. Robert Wood Johnson Foundation and Urban Institute. [Online] April 2017. https://www.urban.org/sites/default/files/publication/89986/2001246_the_cost_of_not_expanding_medicaid_updated_analysis.pdf.
- Fox, William, Harris, Matthew and Murray, Matthew. Who Benefits Under Insure Tennessee? UT Center for Business and Economic Research (CBER). [Online] January 2015. http://cber.haslam.utk.edu/pubs/bfox304.pdf.
- U.S. Census Bureau. 2012-2016 American Community Survey 5-Year Estimates. [Online] 2017. Accessed via https://factfinder.census.gov/faces/nav/jsf/pages/index.xhtml.
- Tennessee General Assembly Fiscal Review Committee. Corrected Fiscal Note for SJR 93. [Online] March 30, 2015. http://www.capitol.tn.gov/Bills/109/Fiscal/SJR0093.pdf.
- 3-Star Health Task Force. Grey Paper. [Online] June 30, 2016. Obtained from the office of Rep. Cameron Sexton. https://www.sycamoretn.org/wp-content/uploads/2018/03/3-Star-Pilot-Grey-Paper.pdf.
- Antonisse, Larisa, et al. The Effects of Medicaid Expansion under the ACA: Updated Findings from a Literature Review. Kaiser Family Foundation. [Online] September 25, 2017. https://www.kff.org/medicaid/issue-brief/the-effects-of-medicaid-expansion-under-the-aca-updated-findings-from-a-literature-review-september-2017/.
- Miller, Sarah and Wherry, Laura. Health and Access to Care during the First 2 Years of the ACA Medicaid Expansions. New England Journal of Medicine. [Online] March 9, 2017. http://www.nejm.org/doi/full/10.1056/NEJMsa1612890.
- Luna, LeAnn and Pratt, Emily. The Impact of TennCare: A Survey of Recipients, 2017. University of Tennessee Center for Business & Economic Research. [Online] September 2017. http://cber.haslam.utk.edu/tncare/tncare17.pdf.
- Hing, Esther, Decker, Sandra and Jamoom, Eric. Acceptance of New Patients With Public and Private Insurance by Office-Based Physicians: United States, 2013. U.S. Centers for Disease Control and Prevention National Center for Health Statistics. [Online] March 2015. https://www.cdc.gov/nchs/data/databriefs/db195.pdf.
- U.S. Department of Health and Human Services (HHS). 2015 Actuarial Report on the Financial Outlook for Medicaid. Centers for Medicare and Medicaid Services, Office of the Actuary. [Online] 2015. https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/ActuarialStudies/Downloads/MedicaidReport2015.pdf.
- Cassidy, Christina. Rising Cost of Medicaid Expansion is Unnerving Some States. The Associated Press. [Online] October 5, 2016. https://apnews.com/4219bc875f114b938d38766c5321331a/rising-cost-medicaid-expansion-unnerving-some-states.
- U.S. Department of Health and Human Services (HHS). 2016 Actuarial Report on the Financial Outlook for Medicaid. Centers for Medicare and Medicaid Services, Office of the Actuary. [Online] 2016. https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/ActuarialStudies/Downloads/MedicaidReport2016.pdf.
- Avalere Health. Profile of the Medicaid Expansion Population: Demographics, Enrollment, and Utilization. [Online] January 2018. http://go.avalere.com/acton/attachment/12909/f-0517/1/-/-/-/-/Avalere%20Medicaid%20Expansion%20Analysis.pdf.
- Wen, Hefei, Druss, Benjamin and Cummings, Janet. Effect of Medicaid Expansions on Health Insurance Coverage and Access to Care among Low‐Income Adults with Behavioral Health Conditions. Health Services Research. [Online] December 2015. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4693853/.
- U.S. Government Accountability Office (GAO). Behavioral Health: Options for Low-Income Adults to Receive Treatment in Selected States. [Online] June 2015. http://www.gao.gov/assets/680/670894.pdf.
- Tennessee Department of Mental Health and Substance Abuse Services. Presentation to House Health Committee. [Online] February 6, 2018. Via http://tnga.granicus.com/MediaPlayer.php?view_id=379&clip_id=14290.
- Lindrooth, Richard, et al. Understanding The Relationship Between Medicaid Expansions And Hospital Closures. Health Affairs. [Online] January 2018. https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2017.0976.
- Hinton, Elizabeth, et al. Section 1115 Medicaid Demonstration Waivers: The Current Landscape of Approved and Pending Waivers. The Kaiser Family Foundation. [Online] December 13, 2017. https://www.kff.org/medicaid/issue-brief/section-1115-medicaid-demonstration-waivers-the-current-landscape-of-approved-and-pending-waivers/.
- Neale, Brian. Kentucky Medicaid Waiver Approval Letter. Centers for Medicare and Medicaid Services. [Online] January 2018, 12. https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/ky/ky-health-ca.pdf.
- Buntin, Melinda. Memo: HSAs, Cost-Sharing, Wellness Incentives, and Enforcement in 1115 Waiver Programs. Vanderbilt University Department of Health Policy. [Online] November 17, 2016. https://medschool.vanderbilt.edu/health-policy/featured-publications-presentations-resources-0.
- Buntin, Melinda, Graves, John and Viverette, Nikki. Developing and Implementing Health Savings Accounts in Medicaid: Lessons from Pioneering States. Vanderbilt University Medical Center Deparment of Health Policy. [Online] June 2017. https://www.vumc.org/health-policy/files/health-policy/public_files/Health%20Savings%20Accounts%20in%20Medicaid.pdf.
- —. Cost Sharing, Payment Enforcement, and Healthy Behavior Programs in Medicaid: Lessons from Pioneering States. Vanderbilt University Medical Center Department of Health Policy. [Online] June 2017. https://www.vumc.org/health-policy/files/health-policy/public_files/Cost%20Sharing,%20Payment%20Enforcement,%20and%20Healthy%20Behavior%20Programs%20in%20Medicaid.pdf.
- —. State Medicaid Lessons For Federal Health Reform. Health Affairs. [Online] June 7, 2017. https://www.healthaffairs.org/do/10.1377/hblog20170607.060481/full/.
- Lewin Group. Indiana Healthy Indiana Plan 2.0: Interim Evaluation Report. [Online] July 6, 2016. https://www.in.gov/fssa/files/Lewin_IN%20HIP%202%200%20Interim%20Evaluation%20Report_FINAL.pdf.
- Askelson, Natoshia, et al. Iowa’s Medicaid Expansion Promoted Healthy Behaviors But Was Challenging To Implement And Attracted Few Participants. Health Affairs. [Online] May 2017. https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2017.0048.
- Semanskee, Ashley, Cox, Cynthia and Levitt, Larry. Data Note: Effect of State Decisions on State Risk Pools. The Kaiser Family Foundation. [Online] October 2016. http://files.kff.org/attachment/Data-Note-Effect-of-State-Decisions-on-State-Risk-Pools.
- Sen, Aditi and DeLeire, Thomas. The Effect of Medicaid Expansion on Marketplace Premiums. U.S. Department of Health and Human Services (HHS). [Online] September 6, 2016. https://aspe.hhs.gov/system/files/pdf/206761/McaidExpMktplPrem.pdf.