Key Takeaways
- Defining the goals and details of a potential TennCare work policy, seeking better data, and accounting for obstacles to work and self-sufficiency may help policymakers weigh its full impact.
- A TennCare work requirement could potentially have unintended consequences, including new costs and inefficiencies in state government and the loss of health coverage for some low-income Tennesseans.
The Trump administration has opened the door to letting states require some Medicaid enrollees to work or engage in work-related activities. This report outlines key points to consider for state policymakers who want to add a work requirement to TennCare.
Part 1 in this series examined recent Medicaid work requirement proposals, their policy rationale, and the populations most likely to be affected if implemented in Tennessee. Part 2 summarized Tennessee’s welfare-to-work experience with Families First, the state’s Temporary Assistance for Needy Families (TANF) program. Together, these reports seek to help interested parties weigh the trade-offs of a Medicaid work requirement. Get the whole 3-part series here.
Key Considerations for a Potential TennCare Work Requirement
Tennessee policymakers thinking about adding a work requirement to TennCare may want to consider the following issues in order to weigh the full impact of such a policy change.
Defining the Goals
State policymakers may want to carefully consider and articulate their goals for a Medicaid work requirement. Defining the overarching goals and the problem to be solved will help policymakers to weigh the potential benefits against the potential costs. This may help to determine whether TennCare is the most cost-effective mechanism for achieving their goals and, if so, how best to measure and track the policy’s effectiveness.
Details of the Work Requirement
Medicaid work requirements proposed by other states vary in significant ways. Questions Tennessee policymakers would need to answer include: Who is subject to a work requirement? How would TennCare consider individual health challenges that may impact the ability to get and/or maintain employment (e.g. chronic physical or mental health issues, substance use disorders)? What qualifies as a work activity? Are work activities a condition of eligibility? How does eligibility change for individuals who gain employment? What exemptions would be made for caregiver duties or other circumstances? How will the work requirement be phased into the current program? Can TennCare support employment without a work requirement (e.g. supportive employment services, referrals to job training and job search programs)? (1)
Limitations of Existing Research
Existing research on Medicaid coverage’s effect on the labor market has important limitations. We are not aware of any studies that measure the impact of a Medicaid work requirement on individuals’ incomes, access to health care, or metrics of overall well-being. In addition, existing studies of employment impacts (including one on Tennessee’s 2005-2006 disenrollment) only explore populations that are not currently eligible for TennCare.
Legal Questions
A potential new TennCare work requirement may face legal challenges. Some have questioned whether the federal government can legally authorize states to implement work requirements without an explicit change in law by Congress. (2) Media reports indicate that organizations that litigate over health issues are likely to sue if state requests to add work requirements to Medicaid are approved. (3)
Better Data for Planning
Better data about non-elderly, non-disabled TennCare enrollees could yield useful insights. Tennessee has not opted into the Affordable Care Act’s optional Medicaid eligibility expansion, so childless adults without disabilities are largely ineligible for TennCare. The data presented in Part 1 provide a snapshot of the work status of non-elderly adults who are enrolled in TennCare. However, key information is missing about enrollees’ specific health conditions, circumstances, and reasons for not working.
Support Services
Some TennCare enrollees may need help to make work feasible. Child care, transportation, education, and training needs, along with job offerings and work-related expenses, can all make it harder to get, keep, and advance in a job. (4) (5) Families First provides support in each of these areas. The adult TennCare population is much larger, more medically-complex, and with higher work rates — a product of TennCare’s higher income eligibility standards. Services that may fit Families First would likely need changes to accommodate the TennCare population.
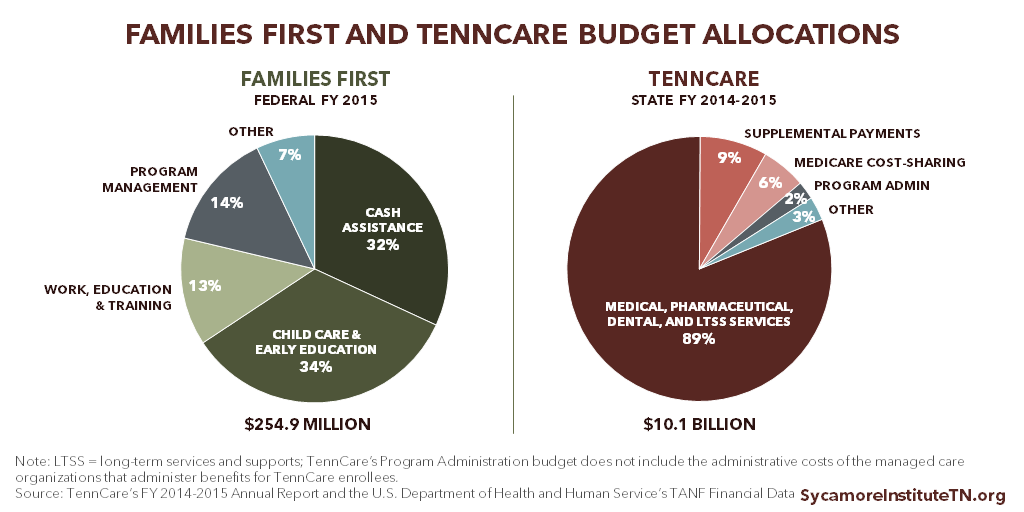
Figure 1
Funding Needs
Support services for a TennCare work requirement may need significant funding. Families First spent 34% of its budget on child care and 13% on work and training services in 2015. (Figure 1). Tennessee policymakers might consider whether and how to leverage or expand existing employment and training support programs to support the goals of a potential TennCare work requirement.
Administrative Burden
A potential TennCare work requirement would necessitate systems changes and increase administrative costs. Implementing and tracking work activities in Families First requires additional staff time, coordination among state agencies and contractors, and infrastructure for offering support services. (8) All of these processes would have to be scaled up and adapted as TennCare serves a much larger population than Families First. Policymakers would need to consider how to implement, monitor, and enforce work requirements in tandem with TennCare’s existing services and responsibilities.
The Countercyclical Nature of TennCare
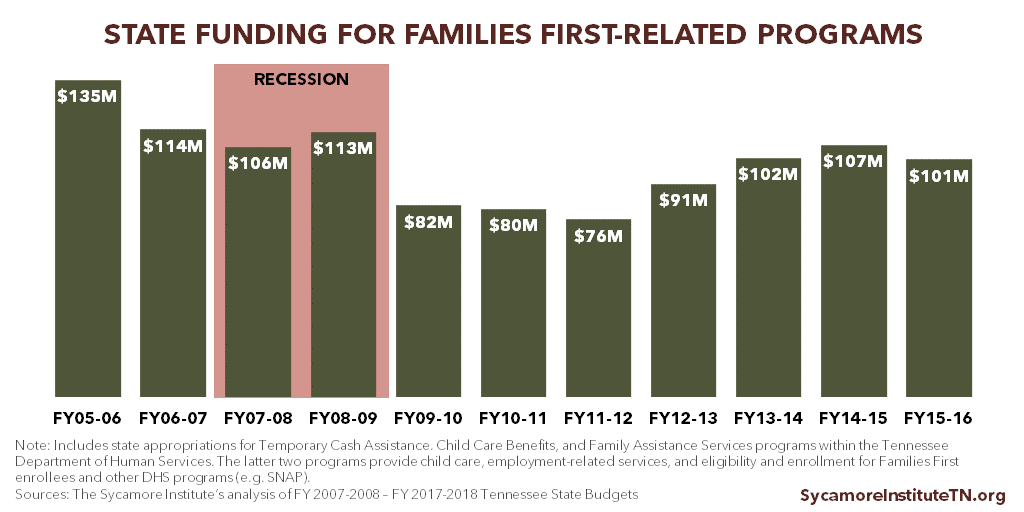
TennCare is a countercyclical program, meaning enrollment goes up during recessions. Job and income losses during economic downturns make more people eligible for TennCare and can make completing work activities more difficult. Economic downturns can also stress state budgets, which may affect state funding of support services for work requirements. In response to the 2007 recession, for example, some states reduced TANF work supports and services. (9) In Tennessee, state funding for Families First-related programs was cut during the recession and the years that followed (Figure 2).
Figure 2
Consistency and Coordination
Some TennCare enrollees who also receive Supplemental Nutrition Assistance Program (SNAP), public housing, or TANF benefits already face work requirements. Medicaid work requirements may overlap with existing efforts, which could create confusion or inconsistency for enrollees and recipients. State policymakers may want to ensure that multiple programs affecting the same populations apply consistent standards and coordinate their support services.
Availability of Jobs
Policymakers may want to consider whether a potential TennCare work requirement accounts for variation in the amount and quality of job opportunities across the state. Some SNAP requirements, for example, can be waived in places with high unemployment or low job availability. (10) Residents of areas with fewer jobs or higher barriers to employment (e.g. transportation or affordable child care) may find it harder to fulfill work requirements and could face greater risk of losing coverage. Rural areas of the state are more likely to have fewer job opportunities and higher rates of TennCare enrollment. In 2016, 21 counties in Tennessee were economically distressed and 33 counties were at risk. (11)
Challenges to Becoming Self-Sufficient
The structure of work requirements and related support services can affect participants’ ability to become self-sufficient. When participants in welfare-to-work programs increase their incomes above certain levels, their benefits often decrease or end (i.e. the “benefit cliff”). If their work-related expenses (e.g. transportation, child care, private health insurance coverage) also go up, these individuals may have continued trouble becoming self-sufficient. (12) Policymakers may want to consider how the structure of work requirements and related supports would influence participants’ overall economic status and well-being.
Out-of-Pocket Costs and Uncompensated Care
A TennCare work requirement could potentially increase out-of-pocket health costs for some low-income Tennesseans, which may lead to more bad debt for hospitals. If individuals who fail to meet work requirements lose Medicaid coverage, their out-of-pocket costs for health care would likely go up. To the extent those bills go unpaid, hospitals’ would face higher costs for uncompensated care. Individuals who instead forgo care altogether could experience negative effects on their health, well-being, and productivity.
Potential Unintended Effects of a TennCare Work Requirement
A TennCare work requirement may help encourage self-sufficiency but could potentially have unintended consequences, including new costs and inefficiencies in state government and the loss of health coverage for some low-income Tennesseans.
Unexpected costs and inefficiencies may result from the administrative and programmatic resources needed for implementation as well as the potential for duplication of similar efforts. For example, the implementation of work requirements in Families First required significant administrative effort and funding for support services.
Some low-income Tennesseans may lose access to health coverage — a driver of health and a tool for self-sufficiency — for reasons policymakers do not intend. For example:
- Some TennCare enrollees may have valid or understandable reasons for not working that a new work policy does not take into account.
- Individuals who qualify for multiple benefits programs with work requirements may be confused about which standards they must meet.
- Some individuals who become ineligible for TennCare as a result of higher incomes from work may not have access to affordable health coverage from their employer or in the individual market. Even with health coverage, some individuals may be unable to afford the cost-sharing requirements of private coverage like deductibles and co-payments.
Lack of adequate health coverage can negatively affect an individual’s health and economic well-being, which could unintentionally reduce their odds of achieving long-term self-sufficiency. Forgoing needed care due to cost may lead to worse health outcomes, an important factor in productivity. In addition, higher out-of-pocket spending could negatively affect an individual’s overall economic status.
Parting Words
Defining the goals and details of a potential TennCare work requirement, along with better data on the affected population, would be essential to any attempt to weigh its full impact. Significant investments in services that support participants’ ability to work may be necessary. If not thoughtfully designed, a TennCare work requirement could also have serious unintended consequences.
More information about Medicaid work requirements and Tennessee’s experience with welfare-to-work programs is available in Part 1 and Part 2 of this 3-part series.
References
Click to Open/Close
- Musumeci, MaryBeth and Zur, Julia. Medicaid Enrollees and Work Requirements: Lessons From the TANF Experience. Kaiser Family Foundation. [Online] August 18, 2017. https://www.kff.org/medicaid/issue-brief/medicaid-enrollees-and-work-requirements-lessons-from-the-tanf-experience/
- National Health Law Program. Medicaid Work Requirements – Legally Suspect. [Online] March 21, 2017. https://healthlaw.org/resource/medicaid-work-requirements-legally-suspect/
- Dickson, Virgil. CMS Overhaul of Medicaid May Face Legal Challenges. Modern Healthcare. [Online] November 7, 2017. http://www.modernhealthcare.com/article/20171107/NEWS/171109900
- Holcomb, Pamela A and Martinson, Karin. Implementing Welfare Reform across the Nation. The Urban Institute. [Online] August 2002. http://www.urban.org/sites/default/files/publication/60196/310551-Implementing-Welfare-Reform-across-the-Nation.PDF
- Freedman, Stephen, et al. National Evaluation of Welfare-to-Work Strategies: Two-year Impacts for Eleven Programs. Manpower Development Research Organization. [Online] June 2000. http://www.mdrc.org/sites/default/files/full_93.pdf
- Tennessee Division of Health Care Finance & Administration. TennCare Fiscal Year 2014-2015 Annual Report . [Online] https://www.tn.gov/assets/entities/tenncare/attachments/tenncareannual1415.pdf
- U.S. Department of Health and Human Services (HHS). TANF Financial Data – FY 2015 (“Tennessee” Table). Administration for Children and Families (ACF) Office of Family Assistance. [Online] September 26, 2017. Accessed via https://www.acf.hhs.gov/ofa/resource/tanf-financial-data-fy-2015
- Medicaid and CHIP Payment and Access Commission (MACPAC). Work as a Condition of Medicaid Eligibility: Key Take-Aways from TANF. [Online] October 2017. https://www.macpac.gov/wp-content/uploads/2017/10/Work-as-a-Condition-of-Medicaid-Eligibility-Key-Take-Aways-from-TANF.pdf
- Hahn, Heather, Kassabian, David and Zedlewski, Sheila. TANF Work Requirements and State Strategies to Fulfill Them. Urban Institute. [Online] March 2012. https://www.acf.hhs.gov/sites/default/files/opre/work_requirements_0.pdf
- U.S. Department of Agriculture (USDA). Supplement Nutrition Assistance Program: Able-Bodied Adults without Dependents. Food and Nutrition Service. [Online] August 29, 2017. https://www.fns.usda.gov/snap/able-bodied-adults-without-dependents-abawds
- Transparent Tennessee. Distressed Counties. [Online] https://www.tn.gov/transparenttn/article/openecd-rural-community-development-distressed-counties-dashboard
- Falk, Gene, McCarty, Maggie and Aussenberg, Randy Alison. Work Requirements, Time Limits, and Work Incentives in TANF, SNAP, and Housing Assistance. Congressional Research Service. [Online] February 2014. http://greenbook.waysandmeans.house.gov/sites/greenbook.waysandmeans.house.gov/files/R43400_gb.pdf
Featured Image at top by Justin Merriman / CC BY-NC 2.0