From the flu to salmonella to COVID-19, major disease outbreaks often focus the public eye on public health. But what does that phrase mean, exactly? This report explains what Tennessee’s public health system does, its role in a globalized world, and how Tennessee funds its public health infrastructure.
Key Takeaways
- Public health is a broad field focused on supporting the health of entire populations and communities.
- Spending upfront to prevent costly outbreaks and chronic diseases may save money in the end, but those savings can be hard to measure or take a long time to produce.
- Our public health infrastructure includes distinct systems at the local, state, federal, and international levels, which often coordinate to halt the spread of infectious diseases.
- Adjusted for inflation, Tennessee spends more per resident on public health today than 20 years ago but slightly less than 10 years ago.
What Is Public Health?
Public health is a broad field focused on supporting the health of entire populations and communities, largely by preventing death and disease. (1) (2) It encompasses work on everything from infectious disease (e.g. Ebola and COVID-19) to chronic disease (e.g. type II diabetes and lung cancer) to public safety (e.g. food, road, and water safety). Since many factors drive population health, the field embraces many approaches to accomplish its goals – from individual services to community interventions to broad public policies.
Many aspects of daily life we take for granted were once innovations in public health. Essential building blocks of public health like sewers and water sanitation are now basic infrastructure in most U.S. communities. Prior to these systems, drinking water contaminated with human waste often caused disease and death – a problem that remains widespread in some parts of the world. (3) Examples of other advances in public health from the last century include:
- Childhood Vaccinations – Less than a century ago, thousands of American children died each year from infectious diseases like polio, measles, and whooping cough. The development and wide availability of vaccines has eradicated smallpox and polio, and deaths and sickness from other vaccine-preventable illness have declined sharply. (4)(5)
- Motor Vehicle Safety – Thanks in part to Rutherford County’s Dr. Robert Sanders, otherwise known as “Dr. Seatbelt,” Tennessee in 1977 became the first state to require all children to ride in car seats. (6) The risk of motor vehicle-related injury and death fell significantly in the wake of this public health intervention and related laws about driving under the influence and wearing motorcycle helmets. (7)(8)
- Improved Dental Health – Tooth decay and poor dental health were much more common before the discovery of water fluoridation. In fact, not having enough teeth was a leading cause of rejection from military service in both world wars. Fluoridation is cheap and effective, reducing the total number of decayed, missing, or filled teeth by 50-70%. (9)
- Safer and Healthier Foods – Foodborne illnesses have become much less common thanks to widespread use of refrigeration, pasteurization, insecticides, and pesticides. A better understanding of nutrition and the ability to track foodborne bacteria like salmonella to the exact factory and batch have also made our food safer. (10)
Each of us does things every day that affect public health. Some are the subject of laws, like the speed at which we drive. Others are voluntary, like getting an annual flu shot. Similarly, health care providers, government agencies, policymakers, nonprofit and faith-based organizations, and private businesses all play a role in public health.
Spending upfront to prevent costly outbreaks and chronic diseases may save money in the end, but those savings can be hard to measure or take a long time to produce. Public health tends to get the most attention when things go wrong, such as an outbreak of infectious disease like COVID-19 or foodborne illness like E. coli. However, the bread and butter of public health is prevention: stop the outbreak before it starts, keep kids from smoking their first cigarette, make sure food is safe to eat, etc. Measuring a return on those efforts is not always simple and often hinges on value judgments.
Like all public policies, decisions about public health involve trade-offs. Communities, states, and nations must weigh their goals for improving health and advancing the common good with their willingness to devote financial resources and constrain what people are allowed to do. Not every community will strike the same balance.
Figure 1
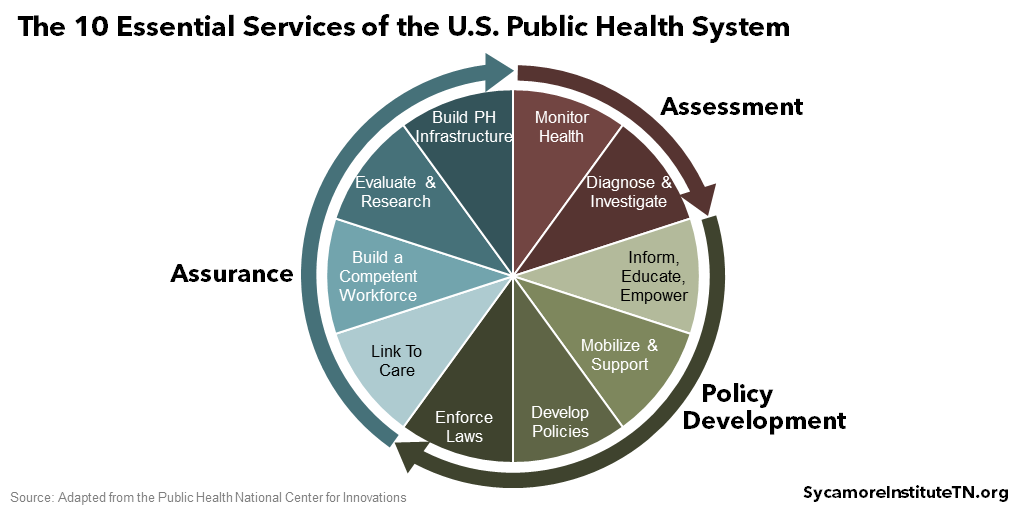
The Cycle of Essential Public Health Services
In the U.S., our public health system provides 10 core services in a cycle of assessment, policy development, and assurance (Figure 1). (11) While the specific services provided by any particular organization will vary, these are generally agreed-upon within the public health field. Originally developed in 1994, the framework was updated in September 2020 to align with current and future public health practice.
Assessment
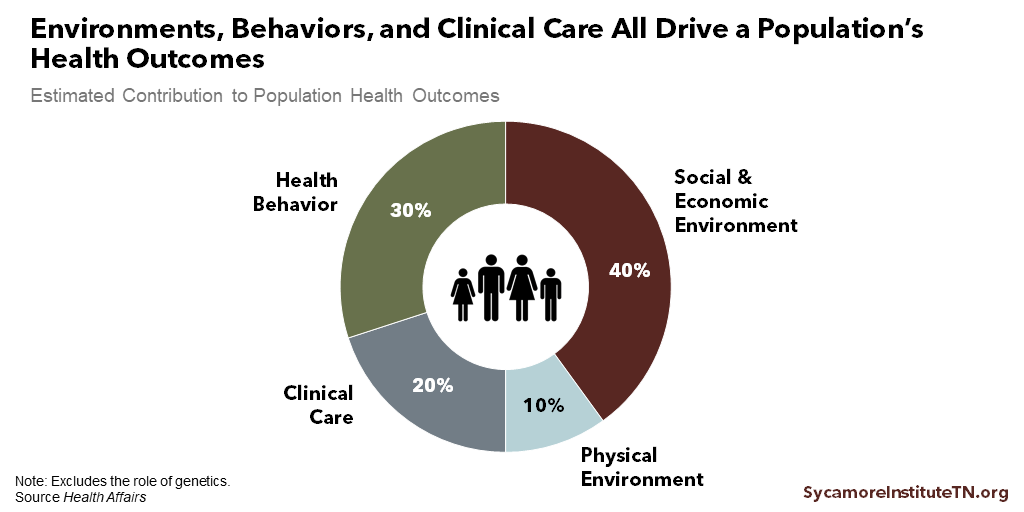
To assess population health, public health systems continually monitor the health of the communities and populations they serve. They also diagnose and investigate the causes of what they find – recognizing that social and economic environments, health behaviors, clinical health care, and physical environment all drive population health (Figure 2).
Policy Development
To address what their assessments uncover, public health officials inform, educate, and empower the communities they serve on the best ways to care for their own health. Due to the many factors that drive health, successful public health efforts often require cooperation across different sectors. They also convene and mobilize community partners to assess and address the community’s needs, develop policies to support community and individual efforts to improve health, and enforce laws and regulations that protect and promote public health.
Assurance
To assure that public health measures are effective and equitable, officials link to care that helps improve health, especially primary and preventative care, and build a competent health care workforce by maintaining safety standards and accreditations. Public health systems also research and evaluate the effectiveness of policies in order to identify best practices and improve efforts to support community health. Finally, they seek to build and maintain a robust infrastructure for improving public health.
Over time, some of our public health system’s activities and focuses have changed. As we made gains in sanitation, food safety, and vaccine-preventable diseases, new challenges took center stage – like chronic disease, behavioral health, and threats of bioterrorism. More recently, upstream factors like community safety, adverse childhood experiences (ACEs), and access to social supports have also gained more attention.
Figure 2
10 Essential Public Health Services in Action
The history of tuberculosis (TB) in the U.S. shows how our public health authorities put their 10 essential services into practice. TB was once a leading cause of death here and continues to cause many deaths around the world. (64)
- Research and Assessment: Decades of research and assessment have revealed how TB spreads, the populations most at risk, and the best treatments.
- Policy Development: That knowledge informs decisions about how to protect the public. For example, Tennessee passed a law in 1971 requiring hospitals to report TB cases to the Dept. of Health. This helped the state deploy resources where they were most needed. (65)
- Assurance: State and local health departments then implement and enforce these policies. For instance, the state health commissioner can require someone with TB to isolate and – if the person refuses to quarantine – detain them until they are no longer infectious.
- More Assessment, Policy, and Assurance: As recently as 2019, the CDC issued new recommendations for TB screening, testing, and treatment of health care personnel. (35) New, drug-resistant forms of TB also require continued research and assessment. And new discoveries will inevitably lead to new policies and assurance activities – continuing the cycle.
Thanks largely to efforts like these, the U.S. had fewer than 9,000 reported TB cases in 2019.
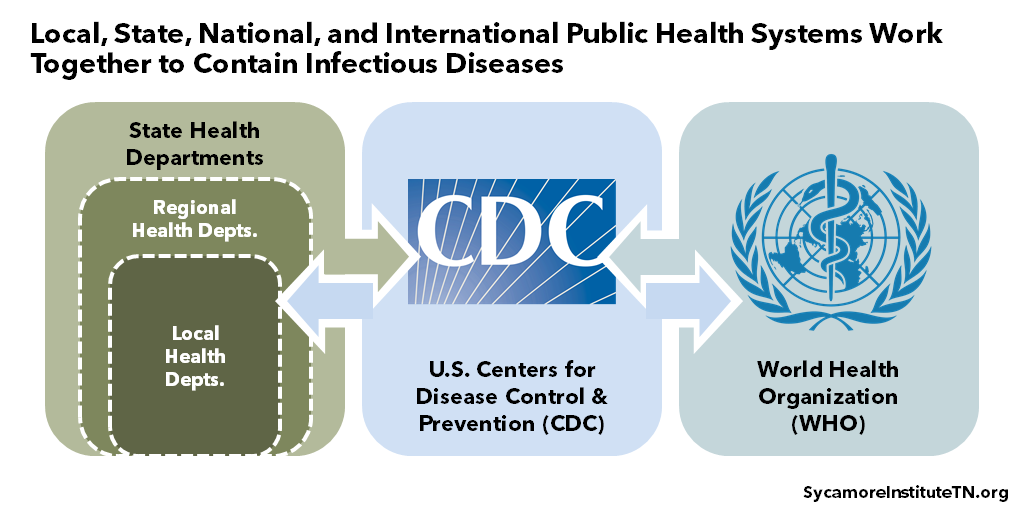
Public Health Infrastructure
Our public health infrastructure includes distinct systems at the local, state, national, and international levels, which often coordinate to halt the spread of infectious diseases (Figure 3). In a globalized world, quick and efficient coordination of data and information is essential to contain disease outbreaks. For this reason, wealthier countries like the United States often share resources and expertise with other parts of the world.
Federal and state laws empower public health systems and policymakers to take extraordinary steps to protect health and safety. For example, they can enforce quarantines, detain those who are suspected to carry communicable disease, and shutdown unsanitary businesses. (13) Specific authorities are discussed below.
Figure 3
State and Local Public Health in Tennessee
The Tennessee Department of Health (TDH) oversees public health in Tennessee. TDH performs all 10 of the essential public health services and also communicates a vision for better health in our state. (14) As part of its responsibilities, TDH:
- Operates eight regional health offices and 89 local county health departments, and supports six independent county public health departments (see below).
- Develops an annual state health plan. For example, the 2019 plan aimed to improve outcomes for people with dementia through better cognitive and brain health across the lifespan. (15)
- Tracks 12 “vital signs” or metrics of Tennesseans’ health. (16)
- Maintains vital records, including birth, death, marriage, and divorce certificates.
- Licenses and regulates health care professionals and facilities.
- Carries out safety inspections of restaurants, pools, hotels, and other establishments.
- Monitors and traces infectious disease outbreaks.
- Implements maternal and child health programs, like the federal Special Supplemental Nutrition Program for Women, Infants, and Children (WIC).
- Operates labs to test bacteria and viruses, environmental samples, and human specimens.(17)
- Conducts prevention activities aimed at decreasing caloric intake, increasing physical activity, and addressing tobacco and substance abuse. (18)
Each of Tennessee’s 95 counties has a local health department. The state operates 89 of them, while Davidson, Hamilton, Knox, Madison, Shelby, and Sullivan counties run their own (Figure 4). (19) This structure is primarily the result of both historical factors and regional dispersion. All 95 bodies may have a locally-appointed Board of Health, and the six locally-run departments still work closely with the state. (20) TDH also has eight regional offices that oversee different regions of the state.
Figure 4

Each local health department tailors its duties to its community’s needs. Local health departments are often the first point of contact for things like vital records and infectious disease outbreaks. Many also provide immunizations, health screenings, restaurant inspections, animal control, and health education programs. In Tennessee, more than half offer comprehensive primary care services as part of the state’s safety net for residents without health insurance – versus about 11% nationwide. (21) The six locally-governed health departments also conduct formal community health assessments to better understand and set priorities in their communities. (22) (23) (24) (25) (26) (27)
State and local officials in Tennessee have the power to act quickly to protect Tennesseans’ health, particularly during a declared emergency. While the federal government can take certain steps to control the spread of disease from abroad and across state lines, states have the primary authority to do so within their borders. (28) Tennessee law lets public health officials take the following actions without prior approval from lawmakers or the courts:
- Quarantines – Under state laws dating back to 1879, Tennessee’s governor, state health commissioner, and county health directors can order quarantines of specific places and individuals from infectious diseases. (29) (30)
- Allocating Resources – During emergencies that involve infectious diseases, state law lets the governor allocate available health care resources to affected areas. (31) Eligible emergencies include those declared by the U.S. president, the governor, or a county. (32)
- Business Closures – County officials can close businesses and other establishments or suspend their license or permit if they’re unsanitary or threaten public health. (30) (33)
- Other Rules & Regulations – Tennessee’s state and local officials have broad power to handle health-related emergencies and dangers. For example, the governor can use executive orders to waive state laws or make people shelter in place. (34) The health commissioner can set rules to prevent infectious disease spread “with the least inconvenience to commerce and travel.” (29) And county health officials can limit any activity that threatens public health and enforce that limit by, for example, revoking or suspending a business license. (33)
Public Health at the National Level
The federal Centers for Disease Control and Prevention (CDC) coordinates public health in the United States and also responds to global health threats. CDC collects and uses data, helps develop public health expertise, grows public health capacity, responds to outbreaks at home and abroad, and operates laboratories. (35) This work supports three broad priorities (35):
- Securing global health and domestic preparedness by responding to pandemics, threats of bioterrorism (e.g. anthrax), and animal-borne diseases (e.g. West Nile Virus and malaria).
- Eliminating diseases like HIV/AIDS, vaccine-preventable illness, and hepatitis C.
- Ending epidemics like those caused by opioids, the flu, and diabetes.
State and local health departments work closely with CDC and rely on its resources to do their jobs. (36) While state and local health departments operate independently, they report death, birth, and other epidemiological data so CDC can observe nationwide trends and adjust resources accordingly. (37) CDC also provides funding, technical assistance, training, data, communications resources, and many other tools. (38)
The federal government can take extraordinary actions to control the spread of diseases from abroad and across state lines. For example, CDC can monitor, detain, and examine people suspected of carrying dangerous communicable diseases into the U.S. or between states. They can also issue quarantine or isolation orders enforceable by local authorities, U.S. Customs and Border Protection, or the Coast Guard. Federal quarantine orders are rare and last occurred during the 1918 influenza pandemic. (13)
Other federal agencies also play important roles in public health. For example, the Department of Health and Human Services (HHS) encompasses CDC, the Food and Drug Administration (FDA), the National Institutes of Health (NIH), the Centers for Medicare and Medicaid Services (CMS), and other agencies. (39) NIH is a major funder of medical research, while FDA regulates the safety of food, medicines, and many other consumable products. (40) (41)
International Public Health
The World Health Organization (WHO) is the branch of the United Nations that oversees and coordinates international public health issues. (42) It provides technical assistance, emergency aid, data collection and research, and health standards for member countries. (43) WHO can also encourage countries to respond to infectious diseases that pose an international threat, like swine flu in 2009, Ebola in 2014, and COVID-19 in 2020. (44)
As a membership organization of nations with different interests and goals, WHO has limited authority. (45) (46) WHO creates norms – not laws – and primarily relies on the cooperation of member states, which may not always occur. (47)
Other organizations also play important roles in international public health. For example, much of the foreign aid the U.S. Agency for International Development distributes goes toward public health in developing countries. (48) Nonprofits and nongovernment organizations like the Bill & Melinda Gates Foundation and Doctors Without Borders also invest in research, programs, and direct medical care to improve health around the globe. (49) (50)
Figure 5

Funding for Public Health in Tennessee
Tennessee spends more per resident on public health today than 20 years ago but slightly less than 10 years ago, adjusted for inflation (Figure 5). (51) (52) (53) (54) The Tennessee Department of Health has a complex and evolving set of responsibilities and funding sources. As a result, trends in the state’s public health spending have at times been skewed by one-time events and changes in state and federal policy. Meanwhile, the department’s responsibilities have grown to include new efforts, such as managing the state’s primary care safety net and addressing the opioid epidemic. The sections that follow provide information and context for understanding TDH’s funding over the last 10-20 years.
In FY 2019, TDH managed over $623 million – primarily from state taxes, health care licensing fees, federal grants, and user and service fees (Figure 6). (51) The department spent this money on four broad functions: public health and health care services, local health departments, health care regulation and licensure, and administration and support.[i] See Table A1 in the Appendix for more detail.
Federal funding accounts for about 38% of TDH’s overall budget, a higher share than most state agencies (Figure 6). In general, federal grants are made for specific purposes and allow less flexibility than state revenue streams. In FY 2019, for example, Tennessee received federal CDC funding for 30 separate projects. (57)
Figure 6

Public Health and Health Care Services
This category includes a wide range of activities, such as laboratory services, maternal and child health, infectious disease response, and the state’s primary care safety net. In FY 2019, nearly half the funding for these activities came from the federal government, 22% from state revenues, and 30% from other sources. (51) (52) (53) (54) The single largest program in this area is WIC, which provides nutrition services and food to low income women and children. WIC funding comes entirely from the federal government and rebates from manufacturers of baby formula (counted as “other revenues”). (51) (55)
Tennessee spent 13% more on public health and health care services in FY 2019 than in FY 2000, adjusted for inflation and population growth (Figure 5). However, funding for these activities varied considerably from year to year. The largest changes were a major state investment to create the primary care safety net after the 2005 TennCare disenrollment and a slow but notable drop in federal WIC funding since about FY 2010 (Figure 7). Since FY 2000, areas with the most significant funding growth have been infectious and environmental disease, emergency preparedness, and family health and wellness. (51) (52) (53) (54)
Local Health Departments
Funding for Tennessee’s local health departments and regional health offices grew steadily over the last two decades, especially from state revenues (Figures 5 and 7). After adjusting for inflation, per capita spending from state dollars for these activities nearly tripled. Some – but not all – of this growth likely came from new funding for local health departments to provide primary care in the mid-2000s. Federal grants also make up about 30% of funding, and nearly one-third comes from other sources like counties and cities, service fees, and funds from other state agencies and/or program line-items. (56) (51) (52) (53) (54)
Figure 7
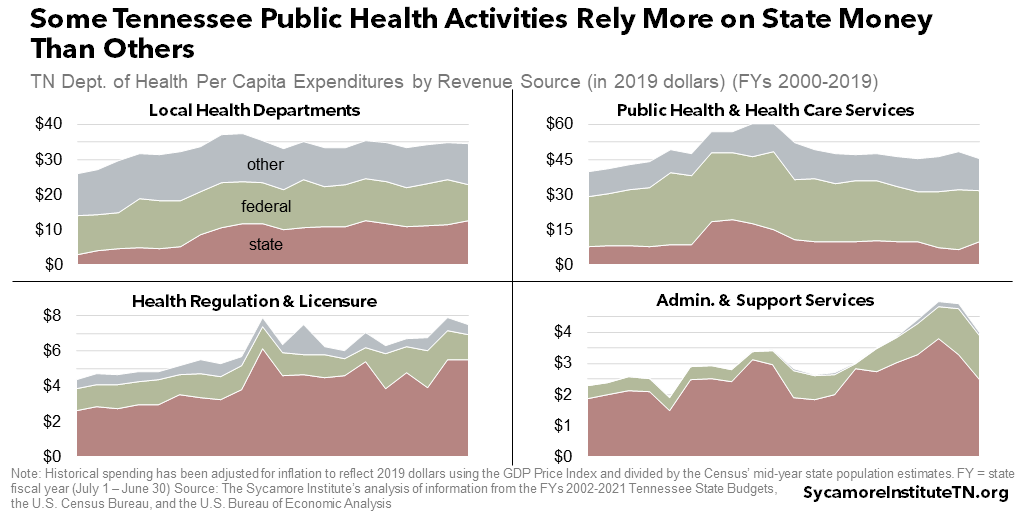
Health Regulation and Licensure
The state’s budget for licensing, regulating, and ensuring the safety of Tennessee’s health care system largely comes from health care providers via state revenues. This category has grown in fits and starts over the last two decades (Figures 5 and 7). The revenue streams include fees from every health professional and facility that is required to have a license or certificate to operate in Tennessee, including physicians, dentists, pharmacists, nurses, midwives, and many others. (51) (52) (53) (54)
Administration and Support Services
The state covers most of the costs for the Department of Health’s administrative functions (Figure 7). These activities include things like management, human resources, and accounting. Spending trends reflect several one-time investments over the years to upgrade technology and data reporting for the statewide public health system. (51) (52) (53) (54)
Trends in Federal CDC Grants
TDH’s inflation- and population-adjusted funding from CDC grew by about 44% over the last decade, but the mix of programs has changed (Figure 8). For example, per capita spending more than doubled during this time for injury and opioid use prevention, immunizations, respiratory and emerging infectious disease activities (e.g. the flu and Zika), and chronic disease prevention. (57) (52) (54)
Tennessee in Context
National studies of states’ public health funding and preparedness show mixed results for Tennessee. Differences in bureaucratic organization and local health departments’ governance and funding structures can make states’ public health efforts tough to compare. For example, an early 2020 analysis put Tennessee in the top tier of states prepared to respond to disease, disaster, and bioterrorism. (58) Meanwhile, definitions of “public health activities” run the gamut – with the most comprehensive including budgets for water and sewer infrastructure and operations. Depending on what’s being counted, Tennessee sits at either the middle or the bottom of the pack for per capita spending on public health. (59) (60) (61) (62)
Figure 8

Parting Words
There are few acts more universally human than to take important things for granted… until they break. Our public health system rarely gets much attention from the general public, yet it performs many functions essential to modern life. Policymakers at every level of government can benefit from understanding what it does, why, and how.
References
Click to Open/Close
- U.S. Centers for Disease Control and Prevention (CDC) Foundation. What is Public Health? [Online] June 14, 2020. [Cited: June 14, 2020.] https://www.cdcfoundation.org/what-public-health.
- The American Public Health Association. What is Public Health? [Online] [Cited: August 12, 2020.] https://www.apha.org/what-is-public-health.
- U.S. Centers for Disease Control and Prevention (CDC). Community Water Systems and Water Safety Plans. [Online] December 17, 2015. https://www.cdc.gov/healthywater/global/community.html.
- —. Achievements in Public Health, 1900-1999 Impact of Vaccines Universally Recommended for Children — United States, 1990-1998. [Online] April 2, 1999. [Cited: June 14, 2020.] https://www.cdc.gov/mmwr/preview/mmwrhtml/00056803.htm.
- —. What Would Happen If We Stopped Vaccinations? [Online] June 29, 2018. https://www.cdc.gov/vaccines/vac-gen/whatifstop.htm.
- Tennessee Highway Safety Office. Child Passenger Safety. [Online] [Cited: August 12, 2020.] https://tntrafficsafety.org/cps.
- U.S. Centers for Disease Control and Prevention (CDC). Achievements in Public Health, 1900-1999 Motor-Vehicle Safety: A 20th Century Public Health Achievement. [Online] May 14, 1999. [Cited: June 2020, 2020.] https://www.cdc.gov/mmwr/preview/mmwrhtml/mm4818a1.htm.
- —. Child Passenger Safety: Get the Facts. [Online] September 13, 2019. https://www.cdc.gov/motorvehiclesafety/child_passenger_safety/cps-factsheet.html.
- —. Achievements in Public Health, 1900-1999: Fluoridation of Drinking Water to Prevent Dental Caries. [Online] October 22, 1999. [Cited: June 14, 2020.] https://www.cdc.gov/mmwr/preview/mmwrhtml/mm4841a1.htm.
- —. Achievements in Public Health, 1900-1999: Safer and Healthier Foods. [Online] October 15, 1999. [Cited: August 12, 2020.] https://www.cdc.gov/mmwr/preview/mmwrhtml/mm4840a1.htm.
- The Public Health National Center for Innovations. 10 Essential Public Health Services. [Online] September 9, 2020. [Cited: September 11, 2020.] https://phnci.org/uploads/resource-files/EPHS-English.pdf.
U.S. Centers for Disease Control and Prevention (CDC). Original Essential Public Health Services Framework. [Online] 1994. [Cited: September 11, 2020.] https://www.cdc.gov/publichealthgateway/publichealthservices/originalessentialhealthservices.html.
- McGovern, Laura, Miller, George and Hughes-Cromwick, Paul. Health Policy Brief: The Relative Contributions of Multiple Determinants to Health Outcomes. Health Affairs. [Online] August 21, 2014. https://www.healthaffairs.org/do/10.1377/hpb20140821.404487/full/.
- U.S. Centers for Disease Control and Prevention (CDC). Legal Authorities for Isolation and Quarantine. [Online] February 24, 2020. [Cited: August 20, 2020.] https://www.cdc.gov/quarantine/aboutlawsregulationsquarantineisolation.html.
- Tennessee Department of Health. Healthier People, Thriving Communities: Our Vision for Tennessee Annual Report 2017. [Online] 2017. [Cited: June 22, 2020.] https://www.tn.gov/content/dam/tn/health/documents/annual-reports/FINAL_2017%20TDH%20Annual%20Report.pdf.
- —. Tennessee State Health Plan- 2019 version. [Online] 2019. [Cited: August 13, 2020.] https://www.tn.gov/content/dam/tn/health/program-areas/state-health-plan/2019-State-Health-Plan.pdf.
- —. Tennessee’s Vital Signs. [Online] [Cited: August 12, 2020.] https://www.tn.gov/health/health-program-areas/tennessee-vital-signs/redirect-tennessee-vital-signs/redirect-dashboard/dashboard.html.
- —. Laboratory Services. [Online] [Cited: August 18, 2020.] https://www.tn.gov/health/health-program-areas/lab.html.
- —. Office of Primary Prevention: 2018/2019 Strategic Plan and Office HIstory. [Online] March 26, 2019. https://www.tn.gov/content/dam/tn/health/program-areas/primary-prevention/OPP_StrategicPlan_2018_19_FINAL_032619.pdf.
- —. Local and Regional Health Departments. [Online] [Cited: June 24, 2020.] https://www.tn.gov/health/health-program-areas/localdepartments.html.
- State of Tennessee. Tennessee Code Annotated § 68-2-601.
- National Association of County & City Health Officials. 2019 National Profile of Local Health Departments. [Online] 2020. https://www.naccho.org/uploads/downloadable-resources/Programs/Public-Health-Infrastructure/NACCHO_2019_Profile_final.pdf.
- Knox County Health Department. Community Health Assessment. [Online] [Cited: August 18, 2020.] https://knoxcounty.org/health/cha.php.
- Metro Health Department. Community Health Assessment. [Online] August 18, 2020. https://www.nashville.gov/Health-Department/Data-and-Publications/Community-Health-Assessment.aspx.
- Shelby County Health Department. Community Health Assessment. [Online] [Cited: August 18, 2020.] http://www.shelbytnhealth.com/264/Community-Health-Assessment.
- Hamilton County Health Department. Community Assessment and Planning (Health Data). [Online] [Cited: August 18, 2020.] http://health.hamiltontn.org/DataMedia/CommunityAssessmentPlanning(HealthData).aspx.
- Sullivan County Regional Health Department. Health Assessment. [Online] [Cited: August 18, 2020.] https://www.sullivanhealth.org/health-assessment.
- Madison County Health Department. 2018 Madison County Community Health Assessment. [Online] [Cited: August 18, 2020.] https://www.madisoncountyhealth.org/uploads/5/9/7/0/59701963/2018_madison_cha_complete.pdf.
- The American Bar Association. Two centuries of law guide legal approach to modern pandemic. [Online] April 2020. [Cited: August 20, 2020.] https://www.americanbar.org/news/abanews/publications/youraba/2020/youraba-april-2020/law-guides-legal-approach-to-pandemic/.
- State of Tennessee. Tennessee Code Annotated § 68-1-201.
- —. Tennessee Code Annotated § 68-2-609.
- —. Tennessee Code Annotated § 68-1-204.
- —. Tennessee Code Annotated § 58-2-101.
- —. Tennessee Code Annotated § 68-2-608.
- —. Tennessee Code Annotated § 58-2-107.
- U.S. Centers for Disease Control and Prevention (CDC). A Bold Promise to the Nation: CDC’s Strategic Framework & Priorities. [Online] Jan 23, 2020. [Cited: June 22, 2020.] https://www.cdc.gov/about/pdf/StrategicPrioritiesReport.pdf.
- —. Public Health Law Program. [Online] [Cited: June 22, 2020.] https://www.cdc.gov/phlp/docs/phl101/PHL101-Unit-1-16Jan09-Secure.pdf.
- —. Defending America from Health Threats. [Online] February 16, 2018. [Cited: June 22, 2020.] https://wwwn.cdc.gov/nndss/how-we-do.html.
- —. Health Department Resources. [Online] March 9, 2020. [Cited: June 22, 2020.] https://www.cdc.gov/publichealthgateway/healthdepartmentresources/index.html.
- U.S. Department of Health and Human Services (HHS). HHS Agencies & Offices. [Online] October 27, 2015. [Cited: June 22, 2020.] https://www.hhs.gov/about/agencies/hhs-agencies-and-offices/index.html.
- National Institutes of Health (NIH). Impact of NIH Research. [Online] [Cited: September 9, 2020.] https://www.nih.gov/about-nih/what-we-do/impact-nih-research.
- U.S. Food and Drug Administration (FDA). What Does the FDA Regulate? [Online] March 28, 2018. [Cited: June 22, 2020.] https://www.fda.gov/about-fda/fda-basics/what-does-fda-regulate.
- World Health Organization (WHO). Constitution of the World Health Organization. [Online] October 2006. [Cited: June 14, 2020.] https://www.who.int/governance/eb/who_constitution_en.pdf.
- Clift, Charles. The Role of the World Health Organization in the International System. Chatham House Publishing. [Online] Chatham House, October 2013. [Cited: June 14, 2020.] https://www.chathamhouse.org/sites/default/files/publications/research/2013-02-01-role-world-health-organization-international-system-clift.pdf.
- World Health Organization (WHO). What are the International Health Regulations and Emergency Committees? [Online] December 19, 2019. [Cited: June 14, 2020.] https://www.who.int/news-room/q-a-detail/what-are-the-international-health-regulations-and-emergency-committees.
- Kupferschmidt, Kai. Mission Impossible? WHO Director Fights to Prevent a Pandemic without Offending China. Science. [Online] February 10, 2020. [Cited: June 14, 2020.] https://www.sciencemag.org/news/2020/02/mission-impossible-who-director-fights-prevent-pandemic-without-offending-china.
- The Associated Press. China Delayed Releasing Coronavirus Info, Frustrating WHO. [Online] June 3, 2020. https://apnews.com/3c061794970661042b18d5aeaaed9fae.
- Lawrence Gostin, Devi Sridhar, Daniel Hougendobler. The Normative Authority of the World Health Organization . Georgetown University Law Center. [Online] 2015. [Cited: June 15, 2020.] https://scholarship.law.georgetown.edu/facpub/1498/.
- U.S. Agency for International Development (USAID). Who We Are. [Online] October 4, 2019. [Cited: June 15, 2020.] https://www.usaid.gov/who-we-are.
- Médecins Sans Frontières/Doctors Without Borders (MSF). Charter. [Online] 2015. [Cited: June 15, 2020.] https://www.doctorswithoutborders.org/who-we-are/principles/charter.
- Bill and Melinda Gates Foundation. What We Do. [Online] [Cited: June 15, 2020.] https://www.gatesfoundation.org/What-We-Do.
- State of Tennessee. FYs 2002-2021 Tennessee State Budget Documents. [Online] 2001-2020. Available from https://www.tn.gov/finance/fa/fa-budget-information/fa-budget-archive.html.
- U.S. Census Bureau. Annual Estimates of the Resident Population for the United States, Regions, States, and Puerto Rico: April 1, 2010 to July 1, 2019 (NST-EST2019-01). [Online] 2020. Accessed from https://www.census.gov/data/tables/time-series/demo/popest/2010s-state-total.html.
- —. Intercensal Estimates of the Resident Population by Single Year of Age and Sex for States and the United States: April 1, 2000 to July 1, 2010. [Online] 2010. Accessed from https://www.census.gov/data/datasets/time-series/demo/popest/intercensal-2000-2010-state.html.
- U.S. Bureau of Economic Analysis . GDP Price Index. [Online] Accessed from https://apps.bea.gov/itable/index.cfm.
- Carlson, Steven, Greenstein, Robert and Neuberger, Zoe. WIC’s Competitive Bidding Process for Infant Formula Is Highly Cost-Effective. Center on Budget and Policy Priorities. [Online] February 17, 2017. https://www.cbpp.org/research/food-assistance/wics-competitive-bidding-process-for-infant-formula-is-highly-cost.
- State of Tennessee. Fiscal Year 2016-2017 Recommended Budget: Expenditures by Object and Funding Source. [Online] 2016. https://www.tn.gov/content/dam/tn/finance/budget/documents/2017ExpRevDetail.pdf.
- U.S. Centers for Disease Control and Prevention (CDC). Grant Funding Profiles: FFYs 2010-2019 Summary Data Download. [Online] [Cited: August 1, 2020.] Accessed from https://fundingprofiles.cdc.gov/Category/Category.
- Trust for America’s Health. Ready or Not 2020: Protecting the Public’s Health from Diseases, Disasters, and Bioterrorism. [Online] February 2020. https://www.tfah.org/wp-content/uploads/2020/01/2020ReadyOrNotFINAL.pdf.
- Weber, Lauren, et al. Hollowed-Out Public Health System Faces More Cuts Amid Virus. Kaiser Health News and the Associated Press. [Online] July 1, 2020. https://khn.org/news/us-public-health-system-underfunded-under-threat-faces-more-cuts-amid-covid-pandemic/.
- State Health Access Data Assistance Center. State Heatlh Compare: Per Person State Public Health Funding, 2019. [Online] [Cited: August 26, 2020.] http://statehealthcompare.shadac.org/rank/117/per-person-state-public-health-funding#2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52/a/27/154/false/highest.
- Trust for America’s Health. The Impact of Chronic Underfunding on America’s Public Health System: Trends, Risks, and Recommendations, 2019. [Online] July 2019. https://www.tfah.org/report-details/2019-funding-report/.
- United Health Foundation. America’s Health Rankings: Public Health Funding – Tennessee. [Online] 2019. [Cited: August 26, 2020.] https://www.americashealthrankings.org/explore/annual/measure/PH_funding/state/TN.
- Global Epidemiology of Tuberculosis and Progress Toward Achieving Global Targets. MacNeil A, Glaziou P, Sismanidis C, Maloney S, Floyd K. s.l. : MMWR Morbidity Mortality Weekly, 2019, Vol. 68. doi.org/10.15585/mmwr.mm6811a3.
- State of Tennessee. Tennessee Code Annotated Title 68, Chapter 9.
Image Credit: Volodymyr Maksymchuk / Shutterstock.com
[i] Our Categorizations
We used the program line-item accounting codes below from the FYs 2002-2021 Tennessee State Budget documents for our four program categories. The line-item names for some of the accounting codes have changed over time. Some activities have also been reorganized into different line-items over time. To the extent that we were able to based on information in the budget documents, however, we made every effort to group line-items so that each category represents the same set of activities over time.
- Public Health and Health Care Services: 343.08 (Laboratory Services), 343.20 (Public Health Policy, Planning, and Informatics), 343.39 (Environmental Health), 343.45 (Health Services Administration), 343.48 (Maternal and Child Health), 343.49 (Communicable and Environmental Disease and Emergency Preparedness), 343.51 (Disease Prevention and Health Promotion), 343.52 (Community and Medical Services), 343.53 (Women, Infants, and Children – WIC)
- Local Health Departments: 343.60 (Local Health Services)
- Health Regulation and Licensure: 343.05 (Health Licensure and Regulation), 343.06 (Trauma System Fund), 343.07 (Emergency Services), 343.10 (Health-Related Boards)
- Administration and Support: 343.01 (Administration), 343.03 (Bureau of Administrative Services), 343.04 (Division of Technology)
We excluded the following programs from historical data for comparability: 343.70 (Nursing Home Resident Grant Assistance Program), 343.44 (Bureau of Alcohol and Drug Abuse Services), 343.09 (Division of Animal Welfare)

