Key Takeaways
- In recent years, Tennessee has made significant investments in a mix of promising, innovative, and evidence-based mental health services and programs for children.
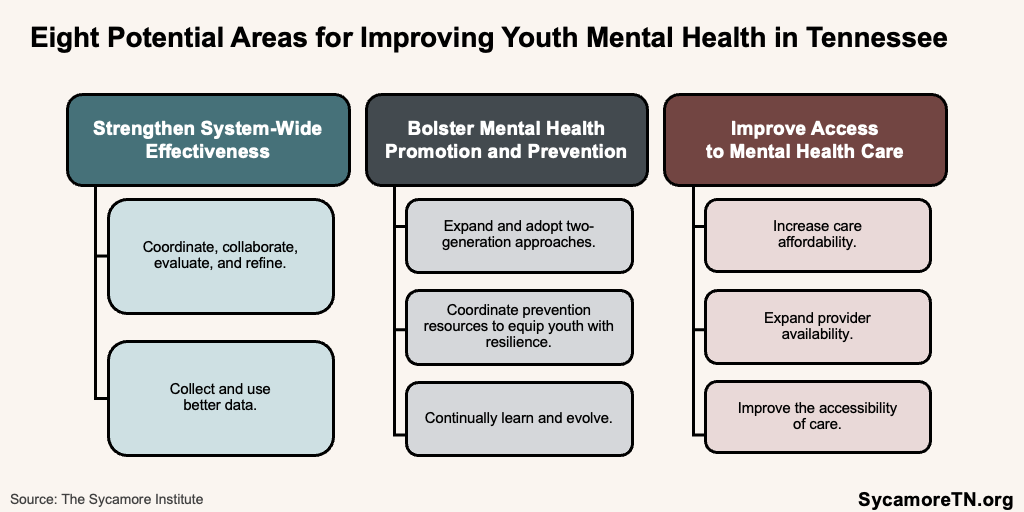
- We identified policy options in eight different areas worth exploring to further strengthen Tennessee’s approach to supporting positive mental health among youth, including:
Strengthen System-Wide Effectiveness
1. Coordinate, collaborate, evaluate, and refine efforts across agencies, systems, and funding sources.
2. Collect and use better data.
Bolster Mental Health Promotion and Prevention
3. Expand and adopt two-generation approaches.
4. Coordinate prevention resources to equip youth with resilience.
5. Continually learn and evolve.
Improve Access to Mental Health Care
6. Increase care affordability.
7. Expand provider availability.
8. Improve the accessibility of mental health care.
Children and youth are struggling with anxiety, depression, and other symptoms of poor mental health. The latest data show that 17.7% of Tennessee adolescents ages 12-17 reported having anxiety or depression in 2021-2022—just above the national rate of 17.1% (Figure 1). (1) Meanwhile, significantly more Tennessee youth have died by suicide in the last decade than in prior decades (Figure 2). Over the 2018-2022 period, Tennessee’s youth suicide death rate was just above the national rate (Figure 3). (2)
This report is the final in our introductory series on child mental health in Tennessee. The first compiled available data on mental health among Tennessee youth. The second summarized Tennessee’s many steps to address these concerning statistics. This report explores policy options in eight areas that state policymakers and program administrators could explore to build on these recent initiatives (Figure 4).
Figure 1
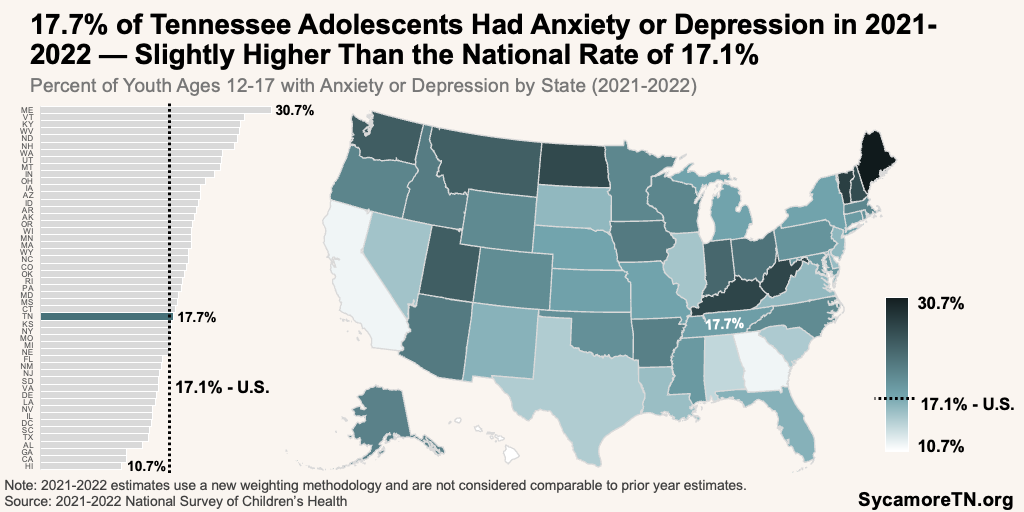
Figure 2
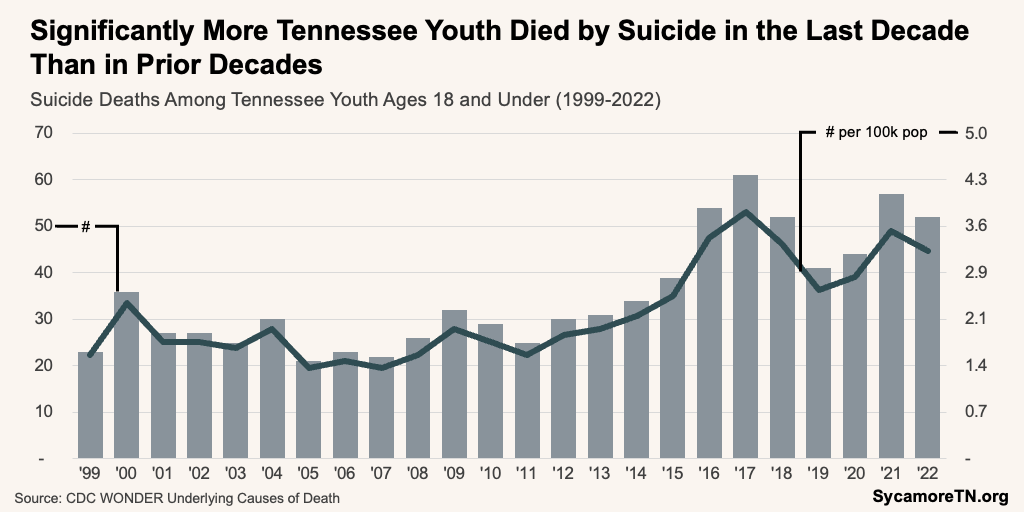
Figure 3
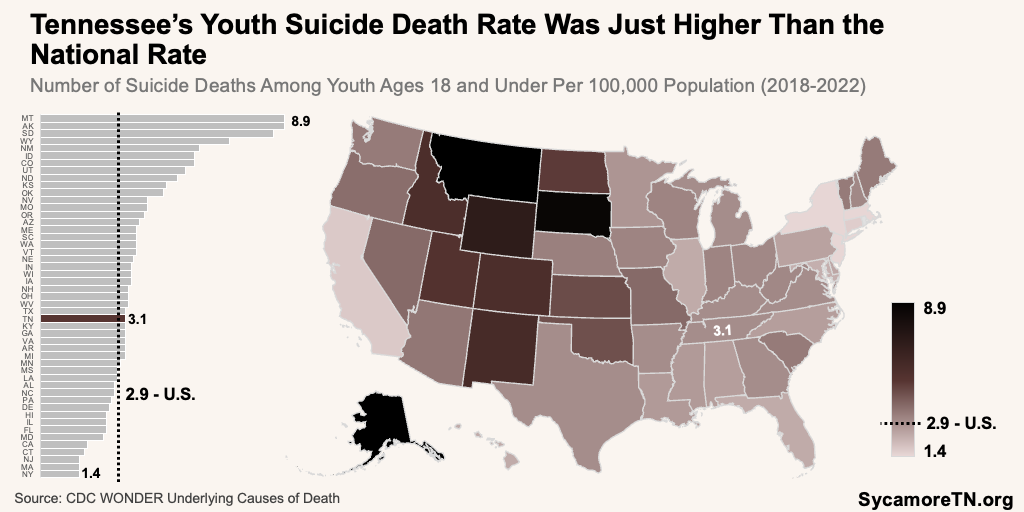
Figure 4
Background
In recent years, Tennessee has made significant investments in a mix of promising, innovative, and evidence-based mental health services and programs for children. Examples include:
- Using new and dedicated funding sources to bolster programming—including a new K-12 Mental Health Trust Fund and shared savings dollars available through Medicaid.
- Removing a requirement that behavioral health services be in a student’s individualized education plan (IEP) for a school to be reimbursed by Medicaid (i.e., TennCare).(3) (4)
- Issuing guidance to schools on assessing and addressing student mental health needs, providing telehealth, and billing for TennCare services. (5)(6) (4) (7) (8) (9)
- Increasing reimbursement rates for community mental health centers.
- Funding tuition assistance to increase the behavioral health workforce.(10)
- Growing the number of youth crisis stabilization units.(11)
- Creating and growing the number of school-based behavioral health liaisons.
- Expanding the types of mental health providers licensed in other states that can practice in Tennessee under multi-state compacts and reciprocal agreements.(12) (13) (14)
- Hiring an assistant commissioner dedicated to child and youth mental health in the Tennessee Department of Mental Health and Substance Abuse Services (TDMHSAS).(15)
Additional policy levers may be worth exploring to further strengthen Tennessee’s approach to supporting positive mental health among youth (Figure 4). Tennessee has already taken many actions in these areas, highlighted throughout and in our previous report. The options discussed here represent additional approaches used or proposed elsewhere or where Tennessee could expand its existing efforts. These options are not necessarily comprehensive, and in many cases, the cited sources can provide more detailed information on the approach or policy.
Figure 5
Strengthen System-Wide Effectiveness
1. Coordinate, collaborate, evaluate, and refine.
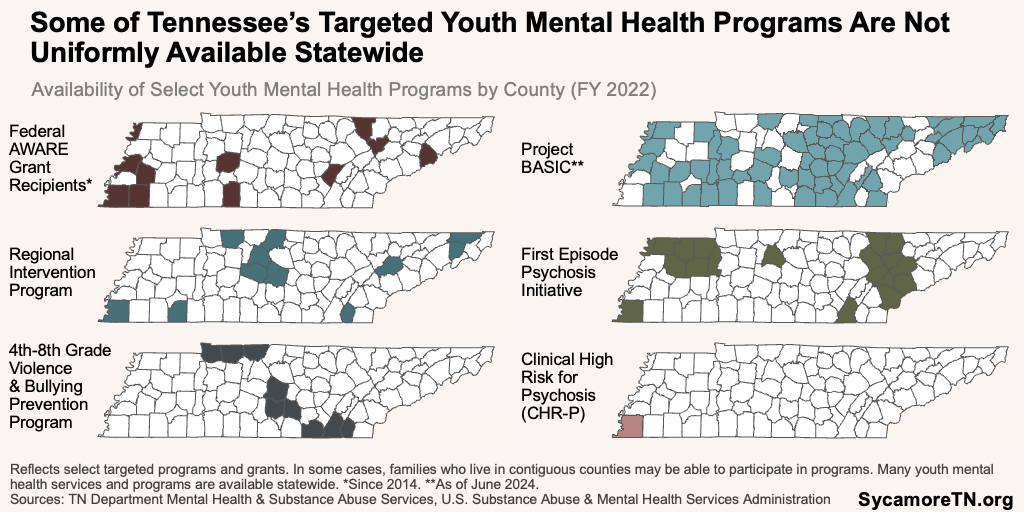
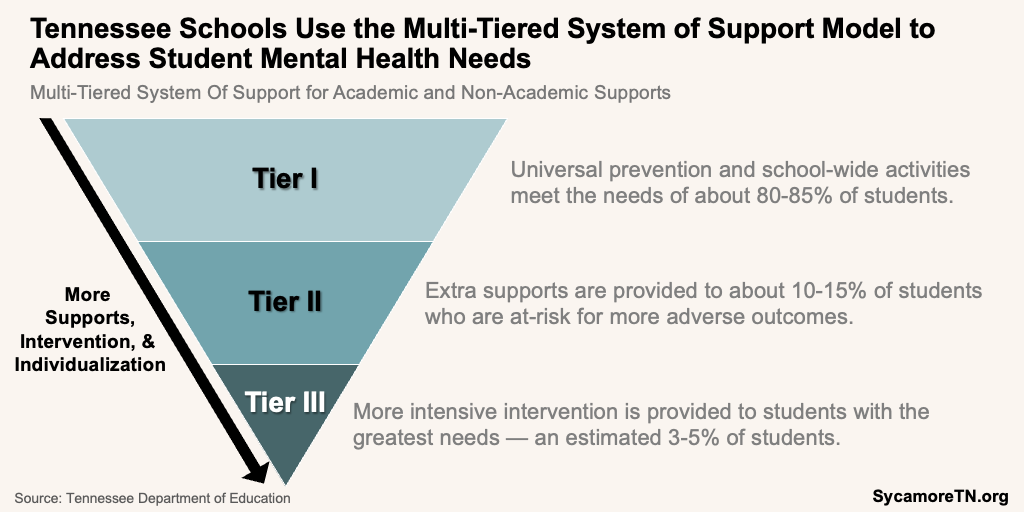
Tennessee’s current efforts to address youth mental health—spread across nine agencies and dozens of programs—may create hurdles for achieving meaningful progress. For example, many laws, regulations, and guidances govern separate but related youth mental health activities, which could be confusing or too restrictive to meet local needs. (22) Some small, time-limited, and/or targeted programs and grants have also not reached all counties (Figure 5)—potentially creating geographic gaps in access to effective programs. Different agencies and programs target different sectors, so partners working in different settings may not always use the same technical language. Meanwhile, information about strategies and outcomes is not always available. For example, a 2023 survey of school districts found that only 37% of responding districts measured outcomes for services provided in all three intervention tiers (Figure 6). (22)
Figure 6
Recent actions create an opportune time to formally and transparently coordinate efforts. As the state rolls out new initiatives and expansions across multiple agencies, policymakers could consider how to bring together all stakeholders to clearly articulate a standard set of measurable outcomes the state hopes to achieve, rigorously evaluate efforts, and continuously adapt. Flexible and dedicated funding sources uniquely position Tennessee to fill gaps, blend disparate funding sources, and offer flexibility to meet distinct and emerging needs. (24)
Coordinate and Collaborate
Tennessee could create a strategy to bring together all relevant agencies and school- and community-based partners to plan, coordinate, and communicate its youth mental health efforts. For example, the state could create a single coordinating entity by revamping existing related vehicles—like Student Support Collaboratives or the Council on Children’s Mental Health. Similar efforts in other states have also included an overarching strategic plan and unified, cross-agency websites that consolidate information, milestones, and data on efforts, programs, and progress. (25) (26) (27) (28) Together, these actions could clarify the state’s objectives, map resources, aid collaborative decision-making, reveal synergies and inconsistencies, clarify key contacts and agencies responsible for specific efforts, help with regional coordination, and address terminology barriers between sectors (e.g., community, medical, and school). (22) (29)
Evaluate and Refine
These efforts could include a comprehensive review of programs, funding, statutes, regulations, and guidance related to youth mental health across all agencies and systems. This—along with rigorous program evaluation—could help all involved stakeholders identify and clarify: (6) (30) (22) (31) (32) (33) (25) (34) (35) (36) (5) (37) (38) (39) (40) (41)
- The outcomes current programs and policies are producing.
- How frontline providers and staff implement existing programs, policies, and practices.
- Areas to align requirements or guidance with the state’s overarching goals for youth mental health, including lessons learned and approaches shown to be effective.
- Gaps in programming across tiers of support and/or geography.
- Ways to better leverage existing resources.
- Programs and requirements with similarities, overlap, duplication, or inconsistencies.
- Disparate funding sources with related goals that could be better coordinated, aligned, braided, or consolidated.
- Opportunities to offer flexibilities to meet local and individual needs.
- Strategies to streamline access to programs and services (i.e., no-wrong-door).
- Roles and responsibilities of the disparate providers and staff positioned to deliver mental health services in school and community settings (e.g., school counselors, school social workers, school psychologists, school-based behavioral health liaisons).
- Needed state-level infrastructure, supports, or incentives to help schools, providers, and communities adopt and deliver effective programs and approaches (e.g., payment incentives, accountability metrics, new guidance, technical resources).
- Activities that could draw down additional federal funds if covered by TennCare.
Evaluating grant-dependent programming could also reveal opportunities to expand effective efforts strategically. State and federal grants fund many mental health services and programs, but they are not all universally available (Figure 5). Reviewing these programs could help the state understand the outcomes each program has delivered and how it might best support the expansion of those that are effective but geographically- or time-limited. For example, do all communities or settings have the capacity and expertise to implement successful programs? Are there opportunities to shift effective grant-funded programs to more systemic or diversified funding models (e.g., insurance reimbursement)? What nudges might best get different partners (e.g., schools, private providers) to integrate successful approaches into ongoing practice (e.g., guidance, mandates)? (22) (30) (32) (40) (24)
These efforts could foster continuous quality improvement, accountability, and performance excellence. Approaches like continuous quality improvement are iterative and often involve using data to consistently and proactively evaluate activities and implementation practices, sharing results, and making program and process refinements. Recognizing and rewarding grantees or communities that achieve notable outcomes could also align programs and local efforts with the state’s objectives, incentivize high performance, and foster a culture of excellence and innovation. This approach would help the state adapt to emerging needs and integrate evidence-based practices more swiftly while supporting partners to work towards common goals. (42) (43) (44) (45) (46)
2. Collect and use better data.
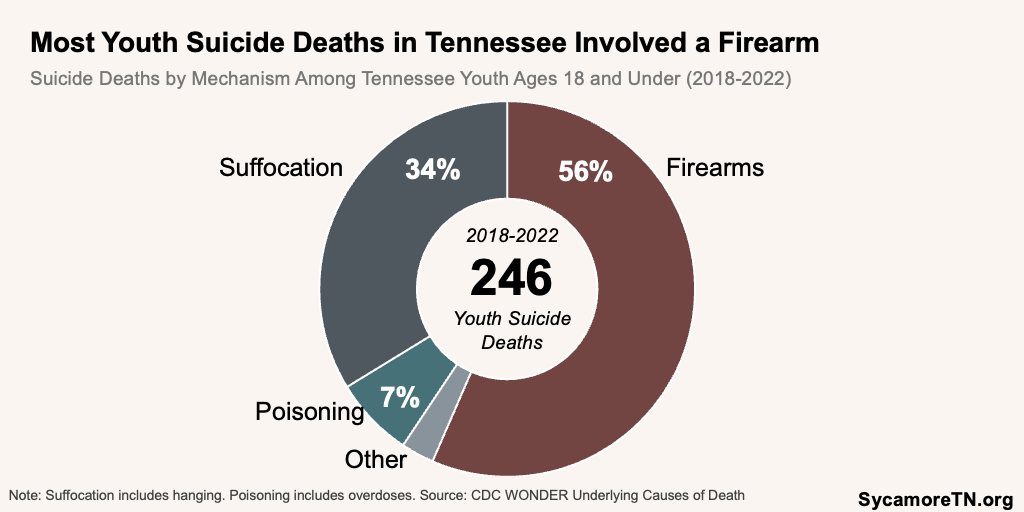
Detailed data can be a useful tool in policy and program planning. For example, death certificates are one of the state’s most comprehensive data sources on health outcomes—available locally and with details on individual characteristics and sometimes circumstances. The 2018-2022 data on youth deaths by suicide show that 56% involved firearms and about a third were by suffocation (most often hanging) (Figure 7). When available, policymakers can use detailed data like this to inform and fine-tune efforts to—for example—reduce the lethality of suicide attempts. (28)
Figure 7
However, the limitations of Tennessee’s current youth mental health data may make it hard to promptly refine and target state and local responses to specific needs. Multiple state and national data sources give insight, but none provide a comprehensive picture of mental health across all ages, demographics, time, or geography. Mental and behavioral health conditions are often defined and gauged differently and grouped together. Detailed mental health care utilization data are not available publicly, and the available data are often published long after collection.
Tennessee could consider state, regional, and local strategies to address gaps in data to understand mental health needs, resources, and service utilization. Ideally, data could provide timely insights on service use in schools and public programs, available resources in each community or region, and child-, school-, and district-level outcomes. Service providers could collect additional metrics to highlight other barriers, such as waitlists and the number of referrals versus providers available in a school, district, county, or region. Collection and reporting would allow for analysis at the local level and across demographic and socioeconomic characteristics and for populations with special needs or higher risks (e.g., intellectual and developmental disabilities). (32) (33) (40) (22) (36) (47) (31) (33)
These efforts could build on or take cues from existing systems in other states and within Tennessee. For example, Tennessee’s P20 Connect is a longitudinal data system that securely links individual-level data across multiple agencies, including K-12 and higher education. (48) Meanwhile, many other states have an all-payer claims database—a repository of health insurance data used to improve health care delivery, transparency, and health outcomes. (49) (50) (51)
Detailed data meeting these criteria could be used for targeted response, program planning, and accountability. For example, schools could use data on chronic absenteeism and school readiness to target efforts for specific students. Resource mapping could help clarify how to access available services and supports for families. Identifying disparities in mental health service use could also highlight where future efforts may have the most impact. Working with state agencies, school districts, and insurers to monitor trends in mental health services, utilization, and outcomes by city, region, and insurance status could help identify potential barriers to care that may not be possible currently. These types of data and activities could help answer questions like:
- Where can children in a region receive needed care regardless of ability to pay?
- How well are needs and access to resources aligned around the state?
- Does the use of school-based services vary by a student’s insurance status?
- How does the use of mental health care differ based on a child or adolescent’s demographic or socioeconomic characteristics?
- Which services, providers, practices, or service settings produce the best outcomes?
Bolster Mental Health Prevention and Promotion
3. Expand existing and adopt new two-generation approaches.
Two-generation approaches integrate services for both child and family and address some of the root causes of poor mental health among youth. For example, the children of parents with poor mental health are much more likely to have worse mental health themselves, and parental needs and behaviors can expose children to toxic stress that contributes to negative outcomes, including poor mental health. Two-generation approaches can address some of these issues in the context of an entire family. (52) (53)
Tennessee could explore ways to expand existing two-generation approaches and find other ways to involve parents in prevention efforts. In FY 2023, over 3,200 Tennessee families across all 95 counties received evidence-based home-visiting services supported by a mix of state and federal dollars. (54) Examples of ways to expand these and other approaches that involve families include: (55) (56) (57) (37) (58) (22) (59) (60) (29) (40) (61)
- Explore TennCare reimbursement and other assistance and incentives to:
- Expand home-visiting.
- Offer parenting programs.
- Increase maternal mental health screenings.
- Integrate screenings for maternal mental health, social service needs, and adverse childhood experiences into pediatric care.
- Combine primary and behavioral health care for new mothers.
- Ensure access to telehealth services—particularly for parents with multiple children in the home.
- Enhance connections between schools and families.
- Provide more mental health resources and literacy for parents and families.
4. Coordinate prevention resources to equip youth with resilience.
School-based mental health prevention activities include a mix of broad efforts supported by the state’s school funding formula and targeted activities funded through special grants. Coordinated School Health—funded through the formula—requires a common set of health services and includes a school counseling, psychological, and social services component, universal prevention, and school-wide activities. Funded by special grants, some schools also offer targeted bullying and suicide prevention programs, trauma-informed practices, and school safety activities that include mental health prevention components.
Tennessee could explore ways to better coordinate narrowly targeted activities to help schools comprehensively address the common drivers of mental health and other concerns like bullying. For example, activities that build and support resilience in children and adolescents can support positive mental health, prevent suicide, and offset the effects of toxic stress that can drive violent behaviors. (62) (63) (64) These include things like trauma-informed practices, safe and supportive environments, meaningful and constructive connections with trusted adults, life skills training, other instruction on coping strategies and self-regulation, and engaging families. (65) (66) (67) (68) (37) (58) Coordinating prevention efforts in this way could help school districts take limited prevention resources further. Additional expansion of these activities into childcare settings could also help identify unique needs earlier, work upstream, and equip new parents with skills and strategies to support resilience.
5. Continually learn and evolve.
As our understanding of the factors that affect youth mental health evolves, so should our policy response. For example, recent efforts to identify root causes have pointed to technology, social media use, increased academic pressure, and even some attempts to increase mental health awareness. Examples of emerging policies and ideas the state might explore include:
- Technology Use — The use of technology comes with trade-offs for youth, and a large body of evidence has shown a connection between youth social media and cell phone use and poor mental health and suicide. (69)(40) (40) (70) (71) (72) Tennessee could explore both innovative and evidence-based policies to address this. For example, some states have adopted statewide school cell phone restrictions. (73) (74) (75) This year, a Tennessee legislative committee rejected a proposed statewide policy, but several schools and school districts across the state have adopted their own. (76) (77) (78) (79) (80) (81) (82) Tennessee could also consider strategies that help youth develop healthy habits outside of school hours, media literacy, and responsible behaviors when using technology (e.g., school-based curriculum, clinician counseling to parents). (83) (84)
- Unintended Consequences of Mental Health Awareness — Some researchers have become concerned that unproven mental health awareness efforts and messaging result in “prevalence inflation.” In other words, youth could be misinterpreting normal levels of stress and anxiety as treatable mental health disorders because of heightened awareness.(85) (86) (87) (88) These potential unintended consequences underscore the need for rigorous evaluation of existing efforts’ effectiveness and investment in evidence-based prevention approaches that build resilience.
- Mental Health Days — As of August 2023, at least 13 states offer excused absences for mental health to help students manage stress and academic pressure.(89) (90) Little research has looked at the effectiveness of mental health days in improving outcomes, but parents have expressed satisfaction with these policies in at least two national surveys. (91) (92) (93) Tennessee could explore this policy—including strategies to pair it with other supports. For example, Delaware requires a referral to a provider after a student has used two excused absences for a mental health reason. (90)
Figure 8
Improve Access to Mental Health Care
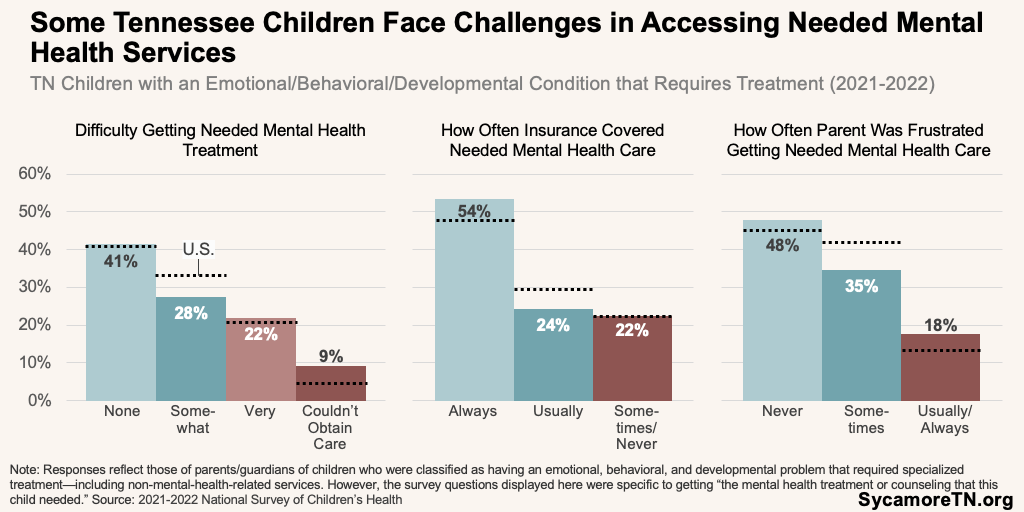
Tennessee recently scored well on a national access to youth mental health services ranking, but challenges remain. In a 2023 data analysis, Tennessee ranked first in the number of mental health treatment facilities and providers serving youth, insurance coverage of behavioral health conditions, and survey results related to cost barriers. (94) However, separate surveys still show that not every child who needs mental health care receives it. In 2021-2022, among Tennessee parents of children with an emotional, behavioral, or developmental condition that required treatment (Figure 8): (1)
- 22% said getting needed mental health treatment for their child was difficult, and 9% said they were not able to obtain care at all.
- 22% said their health insurance plan covered the mental health services that their child needed only sometimes or never.
- 18% responded that they were usually or always frustrated getting the mental health care their child needed.
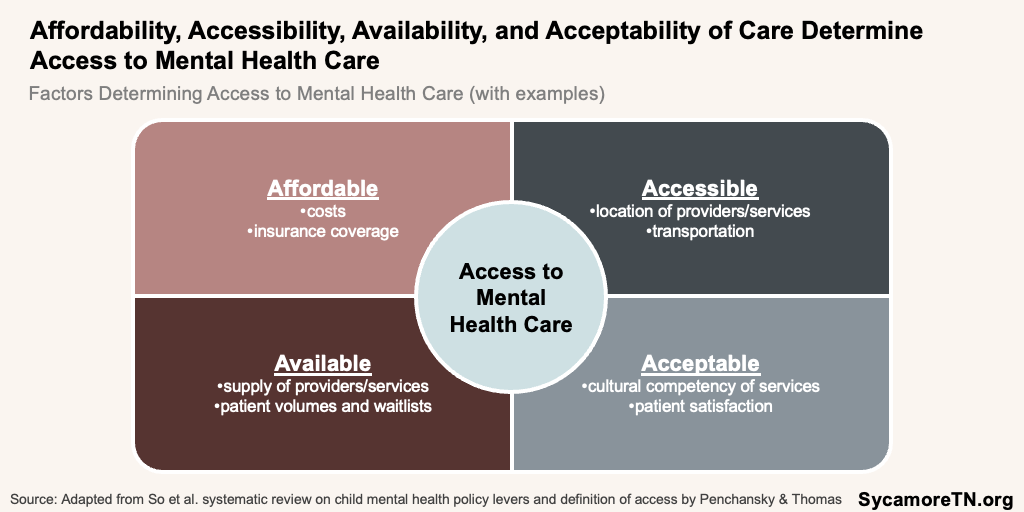
Access to mental health care includes four components—affordability, accessibility, availability, and acceptability (Figure 9). Affordability captures the financial burden of needed services for an individual or family, including health insurance coverage and benefits. Accessibility includes having services conveniently located and/or being able to get to them. Availability encompasses having the right providers and services to meet individual needs, and acceptability is about what people think of the available care. (95) (96) This section focuses on options within the first three of those four components.
Figure 9
6. Increase affordability.
Tennessee could pursue new ways to expand coverage and access to affordable mental health services in public and private plans.
Insurance Coverage Practices
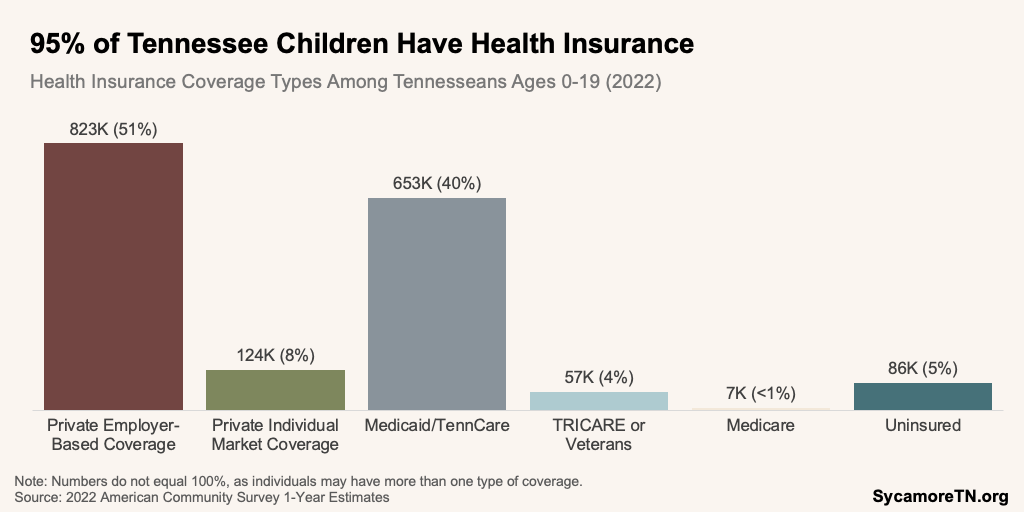
Both public and private health insurance practices affect not only access to care for the children covered by those plans (Figure 10) but also the entire mental health care ecosystem. For example, a long history of coverage limits on behavioral health care created a system in which many private mental health providers do not accept insurance. Insurance policies around covered benefits, provider networks, reimbursement rates, and provider credentialing all influence if and how providers practice and/or contract with plans and offer services. (97) (98) While the state can dictate many Medicaid practices, it could also explore ways to understand and influence private insurer practices by building off federal parity requirements or pursuing an all-payer claims database.
Figure 10
Federal laws and rules provide a regulatory floor for mental health coverage in private and Medicaid health insurance plans. Federal mental health parity law requires most health insurance plans that cover mental health services—including Medicaid—to do so at least as generously as they cover services for physical health. Federal rules proposed in 2023 would enhance that requirement using several new metrics, such as outcome-focused measures and additional evaluations of provider networks and out-of-network reimbursement rates. (100) (101) Meanwhile, new federal Medicaid managed care rules require several steps to ensure access to mental health care—including specific network adequacy standards, secret shopper surveys, and spending analysis. (102)
Tennessee could adopt stronger state-level rules and enforcement mechanisms to ensure that insurance plans provide adequate coverage and access to needed treatment and providers. A new law requires more reporting from the Tennessee Department of Commerce and Insurance on insurers’ coverage and reimbursement rates for behavioral health services. It also requires that TennCare ensure that reimbursement rates for mental health care are on par with those for other benefits. (103) (104) TennCare also has travel time, distance, and wait time requirements for specific behavioral health provider types. (105) Other actions could include:
- Requiring and enforcing stronger minimum network adequacy standards for private plans, which might improve the availability of covered mental health providers.(106) (58) (25) (107)
- Strengthening existing TennCare network requirements, applying them to commercial insurance, and/or studying network adequacy. Other states have, for example, mandated minimum provider-to-enrollee ratios, and some are more specific about how these requirements apply to different individual provider types or services (e.g., differentiated requirements for psychiatrists, psychologists, positive behavioral support, etc.).
- Pairing requirements with more proactive monitoring and enforcement like provider directory reviews, enrollee surveys, secret shopper programs, and quality review activities.(108) (109) (110)
A robust, well-designed all-payer claims database (APCD) could also provide more information about private insurer practices and how they affect children’s mental health care and outcomes. Depending on their design and implementation, APCDs can collect public and private insurer claims data to provide insights on health care utilization, costs, and outcomes for policymakers, insurers, providers, patients, and researchers. Decision makers could use these data to understand differences in coverage practices and payment models and if and how they affect youth mental health care access and outcomes. (51) (111)
EPSDT Coverage
The state could also consider refinements to TennCare’s Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefit. For example, covered children in Tennessee can receive needed mental health services if deemed medically necessary. However, the state could refine its definition of medical necessity to explicitly allow coverage of mental health services without a formal mental health diagnosis. (112) (36) (6) (61) (60) The 2022 Bipartisan Safer Communities Act also requires a federal review of EPSDT implementation across all states by the end of 2024. Any findings from that review can be used to explore additional changes that might increase mental health service access. (38) (113)
TennCare Enrollment
Tennessee has taken many steps to ensure that children enrolled in TennCare keep their coverage. For example, Gov. Lee’s FY 2024 budget funded 12 months of continuous TennCare coverage for eligible kids regardless of income or family size changes—fulfilling a new requirement under federal law. Tennessee has also worked to mitigate coverage losses in the wake of the pandemic. Congress paused routine eligibility redeterminations during the federally declared COVID-19 public health emergency. As those redeterminations restarted in early 2023, Tennessee adopted more federally recommended strategies than any other state to keep eligible children enrolled and—as of April 2024—had seen some of the smallest declines in child enrollment. (114) (115)
However, state officials could also explore additional ways to proactively enroll all eligible children in TennCare. While community mental health centers provide enrollment assistance, other approaches could include equipping schools to participate more actively in outreach and enrollment, marketing campaigns, and using data from other public programs to identify potentially eligible children. (116) (117) (35)
7. Expand availability.
Tennessee could look at additional ways to increase the availability and capacity of mental health care providers.
Public Program Incentives
Tennessee could continue to explore how policies in public programs like TennCare and the behavioral health safety net affect the availability of mental health providers. For example, the state’s FY 2023-2025 budgets included funding to increase reimbursement rates for community mental health centers. The state could continue monitoring how these rate increases affect recruitment and retention, if and how they have affected outcomes, and whether further increases are warranted. (47) (28) TennCare and TDMHSAS could work together to understand if and how Medicaid reimbursement and provider licensing requirements may interact to create barriers to accessing certain services (e.g., facility requirements for telehealth services). TennCare could also explore expanding and/or more specifically stating the different types of providers eligible to bill for mental health services. (118) (61) (47) (29)
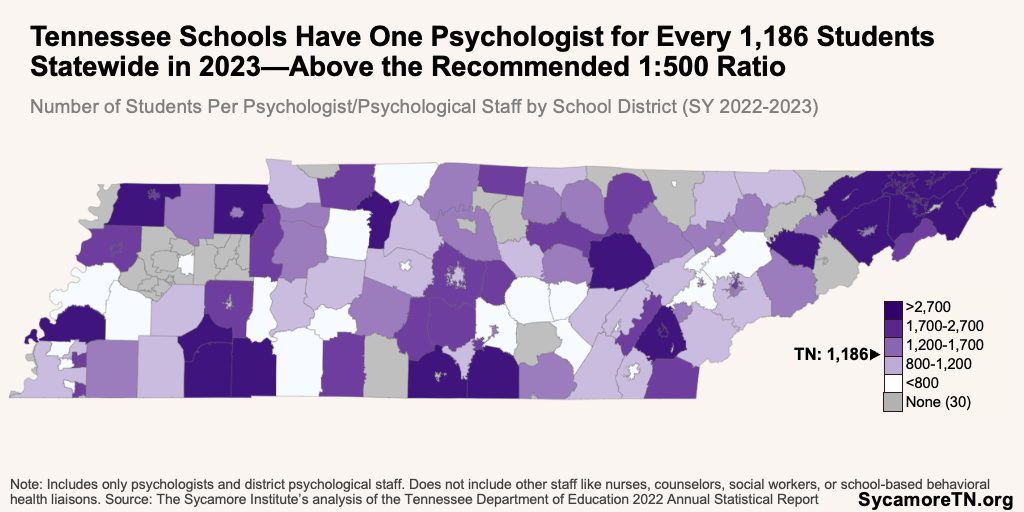
School-Based Provider Ratios and Capacity
Tennessee’s school-based social workers and psychologists serve far more students than is recommended. National organizations recommend one school social worker for every 250 students and one psychologist for every 500 students. (119) (120) In the 2022-2023 school year, only one Tennessee school district met the 1:250 social worker recommendation, and six met the 1:500 psychologist ratio. Statewide, there were 2,689 students for each social worker (Figure 11) and 1,186 for each psychologist and district psychological staff (Figure 12). Half of school districts (70 districts) reported no social workers, and 21% (30 districts) had no psychologists. (121)
Other school-based staff may also position schools to provide mental health services. For example, school nurses and counselors can—to varying degrees—provide some mental health support across the multi-tiered system of supports (MTSS) (Figure 6), while school-based behavioral health liaisons can provide all three service tiers. These staff are available in all Tennessee school districts but not every school. (121) Schools also often have linkages and formal contracts with community-based providers. These many types of providers and resources make it difficult to fully understand each school’s capacity to deliver needed mental health services.
Tennessee could improve the school-based provider-to-student ratios and better understand schools’ capacity to deliver mental health services. Potential approaches include providing targeted grant funding to hire more professionals and/or mandating that school districts meet certain ratio requirements. (107) (122) (123) (37) (35) (124) (22) (39) (40) The state passed a law earlier this year requiring school districts to report on their nurse-to-student ratios. (125) Tennessee could expand the scope of this requirement to explore how each professional role—whether employed by the school or provided through a partnership—delivers mental health services in different school districts. This information could also inform policies that better clarify roles and more effectively deploy limited staff resources across each MTSS tier. (22)
Figure 11
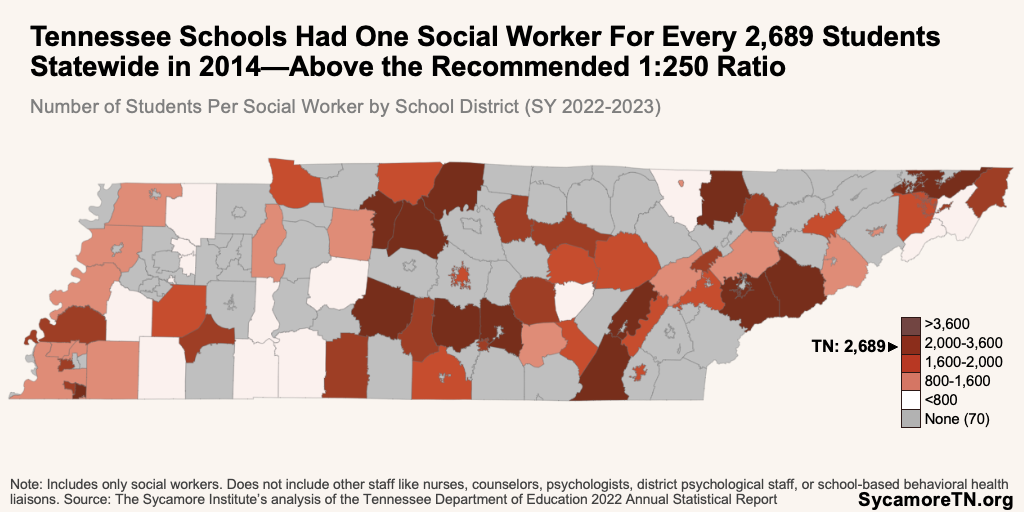
Figure 12
Alternative Roles and Providers
Tennessee could investigate if and how to expand the types of people, roles, and providers that can deliver some mental health messaging, programs, and services. In addition to bolstering prevention, tapping into new roles and providers for lighter-touch services could free up the capacity of existing providers to deliver more advanced levels of care. Examples of strategies that could be explored or expanded:
- A “wellness coach” certification and new bachelor’s degree programs in social work to provide non-clinical mental health services to children and youth.(126) (127)
- Training for community health workers to provide youth mental health services.(128)
- Paraprofessional training and certification.
- More peer-to-peer support, akin to TDMHSAS’ certifications for young adult peer support specialists, to equip older youth to raise awareness, offer coping strategies, and model positive attitudes to one another.(129) (37) (25) (130)
- Required professional development for teachers and other school staff.(22) (31) (131) (107) (35)
- Building on TDMHSAS’ faith-based initiatives to more broadly equip faith leaders with evidence-based practices to raise awareness and support resilience.(132) (58)
- Removing barriers to individual and group telehealth services that remote providers can offer.
8. Improve accessibility.
Tennessee could potentially improve the accessibility of mental health care by taking further steps to integrate behavioral health care into school settings and pediatric primary care.
Integrated Services
Efforts to integrate behavioral health into pediatric primary care and other sources of care can make mental health services more accessible and increase utilization. (95) (68) (6) (133) (58) Outside of ongoing efforts, examples of new approaches could include:
- Provide new or use existing funding to build capacity or provide technical assistance to pediatric practices to provide behavioral health services (e.g., federal maternal and child health block grant). (134) (28)
- Expand, establish, and market new and existing avenues for primary care providers to receive consultation and assistance from behavioral health specialists (e.g., leveraging technology). (36) (26)
- Leverage existing private sector programs that integrate mental health services into pediatric trauma care.(135)
- Explore if and how TennCare reimbursement mechanisms and policies incentivize or create barriers to care integration (e.g., coding systems, enhanced payments, value-based payment incentives, performance metrics, reimbursement for provider-to-provider consultations). (136) (36) (6) (134) (60) (29)
Figure 13
School-Based Health Services
Tennessee can explore ways to expand school-based health services further. (95) Examples of options include:
- Connect schools with the newly created federal technical assistance center on Medicaid school-based service payments. (38)(138)
- Provide TennCare reimbursement for school-based activities like administrative services (e.g., outreach, training, and referral services) and targeted case management.(139) (29)
- Explore if and how to expand the types of providers eligible to provide TennCare-covered services when practicing in the school setting (e.g., special certifications for school health personnel).(5) (29)
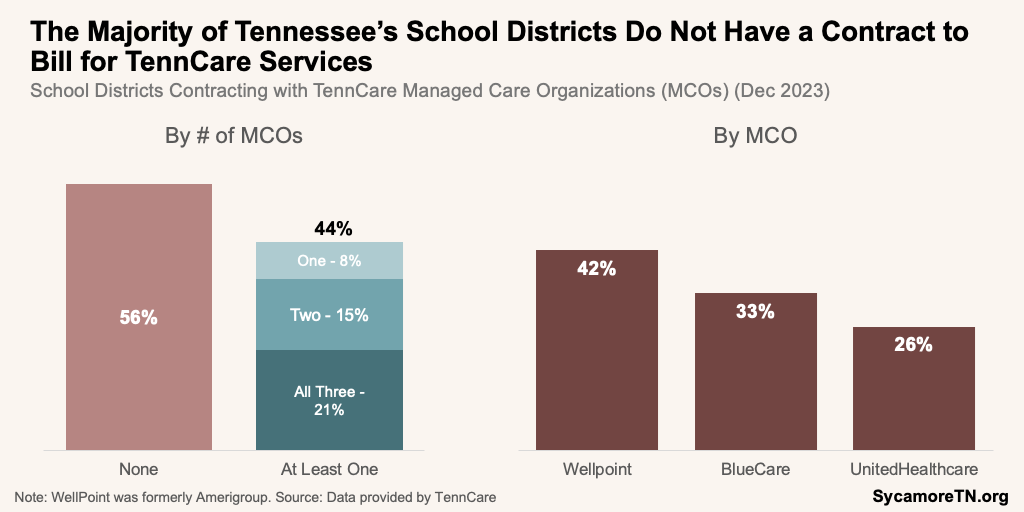
- Test additional approaches for growing the number of school districts that contract with TennCare managed care organizations (MCOs) to receive reimbursement for covered services (e.g., grants to cover the administrative costs of meeting MCO requirements) (Figure 13).
- Explore additional ways to ease the burden schools may face in billing TennCare (e.g., use of an intermediary) or forming linkages with community-based providers.(29)
- Directly involve school personnel and community-based providers practicing in a school setting in decision-making about TennCare reimbursements for school-based services.(5)
- Consider a universal reimbursement schedule for school-based health services across health insurance types to reduce complexity and support the financial sustainability of school-based services.(140)
- Subsidize school districts’ costs for any needed space or technology modifications to offer telehealth services.(28)
- Provide state funding to expand the number of school-based health centers and ensure existing ones can provide mental health care.(30) (141) (37)
Parting Words
Youth mental health indicators have been trending in the wrong direction, highlighting a need for immediate and comprehensive intervention. Tennessee has taken many proactive steps in recent years to meet this need. In this report, we highlight some additional efforts the state could consider to maximize the effectiveness of recent investments in both the short and long term, ensuring a healthy and prosperous future for Tennessee’s children. We encourage readers to explore the cited sources for additional details on each option.
References
Click to Open/Close
- Child and Adolescent Health Measurement Initiative. 2021-2022 National Survey of Children’s Health. Data Resource Center for Child and Adolescent Health supported by the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB). 2024. [Accessed on May 20, 2024.] http://www.childhealthdata.org/. Data are also available from KIDS COUNT Data Center via https://datacenter.aecf.org/.
- U.S. Centers for Disease Control and Prevention (CDC). Multiple Causes of Death Files, 2018-2022 on CDC WONDER Database. National Center for Health Statistics, National Vital Statistics System. 2024. [Accessed on May 20, 2024.] http://wonder.cdc.gov/ucd-icd10-expanded.html. Data are also available from KIDS COUNT Data Center via https://datacenter.aecf.org/.
- Tennessee Commission on Children and Youth. Education: Expand Use of Free Care Rule Reversal Beyond Behavioral Health Services to Cover All Health Services. 2023. https://www.tn.gov/content/dam/tn/tccy/documents/budget-recommendations/fy2025/EducationFreeCare.pdf.
- TennCare and Tennessee Department of Education. TennCare Billing Manual for Tennessee School Districts. https://www.tn.gov/content/dam/tn/tenncare/documents/SchoolBasedServicesBillingManual.pdf.
- Healthy Students, Promising Futures. State Medicaid & Education Standards for School Personnel: A 50-State Review of School Reimbursement Challenges. October 2021. https://healthystudentspromisingfutures.org/wp-content/uploads/2021/11/State-Medicaid-Education-Standards-for-School-Health-Personnel.pdf.
- Frank, Richard G., Wachino, Vikki and Aguilar, Karina. Meeting the Moment on Children’s Mental Health: Recommendations for Federal Policy. USC-Brookings Schaeffer Initiative for Health Policy. December 2022. https://www.brookings.edu/wp-content/uploads/2022/12/20221212_SIHP_ChildrensMHWhitePaperFinal-1.pdf.
- Tennessee Department of Education (TDOE). School-Based Medicaid. https://www.tn.gov/education/families/student-support/special-education/school-based-medicaid.html.
- —. Teleservices Toolkit. June 11, 2020. https://www.tn.gov/content/dam/tn/education/special-education/eligibility/TeleservicesToolkit.pdf.
- —. Tennessee Comprehensive SchoolBased Mental Health Resource Guide. October 2018. https://www.tn.gov/content/dam/tn/education/safety/Comp_School_Mental_Health_Guide.pdf.
- Tennessee Department of Mental Health and Substance Abuse Services (TDMHSAS). Tennessee Behavioral Health Pathways Scholarship. https://www.tn.gov/behavioral-health/scholarship.html.
- —. TDMHSAS Announces Grantees for New Children’s Mental Health Crisis Facilities. May 10, 2024. https://www.tn.gov/behavioral-health/news/2024/5/10/tdmhsas-announces-grantees-for-new-children-s-mental-health-crisis-facilities.html.
- State of Tennessee. Public Chapter No. 700. April 11, 2024. https://publications.tnsosfiles.com/acts/113/pub/pc0700.pdf.
- —. Public Chapter No. 586. March 15, 2024. https://publications.tnsosfiles.com/acts/113/pub/pc0586.pdf.
- —. Public Chapter No. 1041. May 28, 2024. https://publications.tnsosfiles.com/acts/113/pub/pc1041.pdf.
- Tennessee Department of Mental Health and Substance Abuse Services (TDMHSAS). TDMHSAS Announces First-Ever Assistant Commissioner Focused on Mental Health Services for Children and Youth. October 4, 2023. https://www.tn.gov/behavioral-health/news/2023/10/4/tdmhsas-announces-first-ever-assistant-commissioner-focused-on-mental-health-services-for-children-and-youth.html.
- U.S. Substance Abuse and Mental Health Services Administration (SAMHSA). Project AWARE. August 1, 2023. [Accessed on October 1, 2023.] https://www.samhsa.gov/school-campus-health/project-aware.
- Tennessee Department of Education (TDOE). Tennessee Receives Nearly $4.7 Million Project AWARE Grant. November 5, 2021. https://www.tn.gov/education/news/2021/11/5/tennessee-receives-nearly–4-7-million-project-aware-grant-.html#:~:text=Nashville%2C%20TN%20%2D%20Today%2C%20the,Haywood%20County%20Schools%20and%20Scott.
- Tennessee Department of Mental Health and Substance Abuse Services (TDMHSAS). Services for Youth, Young Adults, and Families. [Accessed on August 5, 2023.] https://www.tn.gov/behavioral-health/children-youth-young-adults-families.html.
- Tennessee Commission on Children and Youth (TCCY). Resource Map of Expenditures. 2023. https://www.tn.gov/tccy/programs0/resource-mapping-overview/map-reports.html.
- Tennessee Department of Mental Health and Substance Abuse Services (TDMHSAS). Information provided to the Sycamore Institute about First Episode Psychosis Initiative.
- Information provided. Project BASIC map provided to the Sycamore Institute by the Tennessee Department of Mental Health and Substance Abuse Services on June 20, 2024.
- University of Tennessee Knoxville. Mapping the Landscape of Mental Health Services and Resources for K-12 Students in Tennessee. June 2023.
- Tennessee Department of Education (TDOE). Coordinated School Health. [Accessed on November 1, 2023.] https://www.tn.gov/education/districts/health-and-safety/coordinated-school-health.html.
- State of California. Scaling Evidence-Based and Community-Defined Evidence Practices. Children and Youth Behavioral Health Initiative. 2024. https://cybhi.chhs.ca.gov/workstream/scaling-evidence-based-and-community-defined-practices/.
- Galbreath, Laura, Wilkniss, Sandra and Rohrer, Josh. Behavioral Health System Modernization along the Continuum. National Academy for State Health Policy. March 22, 2024. https://nashp.org/behavioral-health-system-modernization-along-the-continuum/.
- State of California. Governor Newsom’s Master Plan for Kids’ Mental Health. August 2022. https://www.gov.ca.gov/wp-content/uploads/2022/08/KidsMentalHealthMasterPlan_8.18.22.pdf.
- —. Children and Youth Behavioral Health Initiative. 2024. https://cybhi.chhs.ca.gov/.
- State of North Carolina. Investing in Behavioral Health and Resilience: A Comprehensive Plan to Strengthen North Carolina’s Mental Health and Substance Use Disorder Treatment System. March 2023. https://www.ncdhhs.gov/investing-behavioral-health-and-resilience/download?attachment.
- Gratale, Daniella, et al. Fostering School-Based Behavioral Health Services: Innovative and Promising Models, Policies and Practices From Across the Nation. Nemours Children’s Health. September 2023. https://www.nemours.org/content/dam/nemours/shared/collateral/policy-briefs/policy-brief-fostering-school-based-behavioral-health-services-policies-and-practices.pdf.
- Rafa, Alyssa, et al. State Funding for Student Mental Health. Education Commission of the States. March 2021. https://www.ecs.org/wp-content/uploads/State-Funding-for-Student-Mental-Health.pdf.
- Hoover, S., et al. Advancing Comprehensive School Mental Health: Guidance From the Field. National Center for School Mental Health, University of Maryland School of Medicine. September 2019. https://www.schoolmentalhealth.org/media/som/microsites/ncsmh/documents/bainum/Advancing-CSMHS_September-2019.pdf.
- Colorado Health Institute and Partners for Children’s Mental Health. Serving Colorado’s Children: A Financial Map of the Behavioral Health System. March 2020. https://pcmh.org/wp-content/uploads/2020/05/Childrens-Behavioral-Health-Financial-Map-Report.pdf.
- Public Health Informatics Institute. Using Data to Improve Child and Adolescent Mental Health: The Opening Playbook. https://phii.org/course/using-data-to-improve-child-and-adolescent-mental-health-camh-the-opening-playbook/.
- Stagman, Shannon and Cooper, Janice. Children’s Mental Health: What Every Policymaker Should Know . National Center for Children in Poverty. April 1, 2010. https://www.nccp.org/publication/childrens-mental-health-what-every-policymaker-should-know/.
- Stanford, Libby. New Laws Aim to Combat the Youth Mental Health Crisis. Here’s What They Do. Education Week. August 15, 2023. https://www.edweek.org/leadership/new-laws-aim-to-combat-the-youth-mental-health-crisis-heres-what-they-do/2023/08.
- Smith, Sheila, et al. Medicaid Policies to Help Young Children Access Key Infant-Early Childhood Mental Health Services: Results from a 50-State Survey. National Center for Children in Poverty and Georgetown University Center for Children and Families. June 2023. https://www.nccp.org/wp-content/uploads/2024/02/NCCP-Medicaid-Brief_2.27.24.pdf.
- U.S. Centers for Disease Control and Prevention (CDC). Promoting Mental Health and Well-Being in Schools: An Action Guide for School and District Leaders. December 2023. https://www.cdc.gov/healthyyouth/mental-health-action-guide/pdf/DASH_MH_Action_Guide_508.pdf.
- Guth, Madeline and Williams, Elizabeth. The Safer Communities Act: Changes to Medicaid EPSDT and School Based Services. Kaiser Family Foundation. September 6, 2022. https://www.kff.org/policy-watch/the-safer-communities-act-changes-to-medicaid-epsdt-and-school-based-services/#:~:text=The%20Safer%20Communities%20Act%20required,guidance%20every%20five%20years%20thereafter.
- National Academy for State Health Policy. State Approaches to Improve Comprehensive School Mental Health Systems. March 21, 2021. https://nashp.org/state-approaches-to-improve-comprehensive-school-mental-health-systems/.
- U.S. Surgeon General. Protecting Youth Mental Health: The U.S. Surgeon General’s Advisory. U.S. Department of Health and Human Services (HHS). 2021. https://www.hhs.gov/sites/default/files/surgeon-general-youth-mental-health-advisory.pdf.
- State of California. Behavioral Health Ecosystem Infrastructure. Children and Youth Behavioral Health Inititiative . 2024. https://cybhi.chhs.ca.gov/strategic-area/behavioral-health-infrastructure/.
- West Virginia Department of Human Services. Continuous Quality Improvement Plan for Children’s Programs. Office of Quality Assurance for Children’s Programs. December 2023. https://kidsthrive.wv.gov/Documents/December%202023%20Update_CQI_Plan_FINAL.pdf.
- Nevada Department of Health and Human Services. Continuous Quality Improvement. Division of Child and Family Services. https://dcfs.nv.gov/Programs/CWS/CQI/.
- Casey Family Programs. How Did Washington, DC, Develop Its Approach to Meaningful Continuous Quality Improvement? July 14, 2020. https://www.casey.org/dc-cqi/.
- O’Donnell, Brian and Gupta, Vikas. Continuous Quality Improvement. National Library of Medicine. April 3, 2023. https://www.ncbi.nlm.nih.gov/books/NBK559239/.
- Center of Excellence for Infant and Early Childhood Mental Health Consultation. Accountability and Continous Quality Improvement. Georgetown University Center for Child and Human Development. https://https://www.iecmhc.org/tutorials/effective-consultation/mod3-0//tutorials/effective-consultation/mod3-4/.
- U.S. Department of Health and Human Services (HHS) Office of Inspector General. A Lack of Behavioral Health Providers in Medicare and Medicaid Impedes Enrollees’ Access to Care. March 2024. https://oig.hhs.gov/documents/evaluation/9844/OEI-02-22-00050.pdf.
- Miller, Elise. Data: What Is It and How Can It Help Students? State Collaborative on Reforming Education (SCORE). September 28, 2022. https://tnscore.org/data-what-is-it-and-how-can-it-help-students/.
- APCD Council. All-Payer Claims Database: State Efforts. [Accessed on May 21, 2024.] https://www.apcdcouncil.org/state/map.
- —. Informing Health System Change – Use of All-Payer Claims Databases. March 27, 2018. https://scholars.unh.edu/cgi/viewcontent.cgi?article=1063&context=ihpp.
- McAvey, Kevin. Realizing the Promise of All Payer Claims Databases: A Federal and State Action Plan. December 2022. https://www.manatt.com/Manatt/media/Media/PDF/White%20Papers/RWJF_Realizing-the-Promise-of-APCDs_2022-12_d.pdf.
- Ascend. The 2Gen Approach. Aspen Institute. https://ascend.aspeninstitute.org/2gen-approach/.
- U.S. Centers for Disease Control and Prevention (CDC). Mental Health of Children and Parents — A Strong Connection. March 8, 2023. https://www.cdc.gov/childrensmentalhealth/features/mental-health-children-and-parents.html.
- Tennessee Department of Health (TDH). Tennessee Evidence Based Home Visiting: FY 2023 Annual Report. 2024. https://www.tn.gov/content/dam/tn/health/documents/2023%20Home%20Visiting%20Annual%20Report_FINAL.pdf.
- Thompson, Veronnica and Hasan, Anoosha. Medicaid Reimbursement for Home Visiting: Findings from a 50-State Analysis. National Academy for State Health Policy. May 1, 2023. https://nashp.org/state-medicaid-reimbursement-for-home-visiting-findings-from-a-50-state-analysis/.
- Johnson, Kay and Burak, Elizabeth Wright. Medicaid Support for Infant and Early Childhood Mental Health: Lessons from Five States. Georgetown University McCourt School of Public Policy. September 2023. [Accessed on January 10, 2024.] https://ccf.georgetown.edu/wp-content/uploads/2023/09/State-IECMH-Lessons-Learned-FINAL-9-29-23.pdf.
- U.S. Centers for Disease Control and Prevention (CDC). Working Together, We Can Help Children in Rural Communities Thrive. March 8, 2023. https://www.cdc.gov/childrensmentalhealth/features/rural-health.html#print.
- National Governors Association and New Jersey Governor Phil Murphy. Strengthening Youth Mental Health: A Governor’s Playbook. July 2023. https://www.nga.org/wp-content/uploads/2023/07/Strengthening_Youth_Mental_Health_A_Playbook_for_Governors_July2023.pdf.
- Kirby, Jessica and Slone, Sean. Maternal Mental Health: Strategies to Address Societal and Structural Challenges. Council of State Governments. July 2021. https://www.csg.org/wp-content/uploads/sites/7/2021/09/MaternalMentalHealth_Brief_v4.pdf.
- Browning, Lindsey, Hammer, Gretchen and Minnes, Katherine. Behavioral Health. National Association of Medicaid Directors. March 2021. https://medicaiddirectors.org/wp-content/uploads/2021/03/Medicaid-Forward-Behavioral-Health-Report.pdf.
- Tsai, Daniel. CMCS Information Bulletin: Leveraging Medicaid, CHIP, and Other Federal Programs in the Delivery of Behavioral Health Services for Children and Youth. U.S. Centers for Medicare and Medicaid Services (CMS). August 18, 2022. https://www.medicaid.gov/federal-policy-guidance/downloads/bhccib08182022.pdf.
- Mesman, Esther, Vreeker, Annabel and Hillegers, Manon. Resilience and Mental Health in Children and Adolescents: An Update of the Recent Literature and Future Directions. Curr Opin Psychiatry. 2021 Nov 1;34(6):586-592. doi: 10.1097/YCO.0000000000000741. PMID: 34433193; PMCID: PMC8500371. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8500371/.
- Hinduja, Sameer and Patchin, Justin. Cultivating Youth Resilience to Prevent Bullying and Cyberbullying Victimization. Child Abuse & Neglect, Volume 73, 2017, Pages 51-62, ISSN 0145-2134, https://doi.org/10.1016/j.chiabu.2017.09.010. https://www.sciencedirect.com/science/article/pii/S0145213417303411.
- Han, Jin, et al. Resilience to Suicidal Behavior in Young Adults: A Cross-Sectional Study. Sci Rep 12, 11419 (2022). https://doi.org/10.1038/s41598-022-15468-0. https://rdcu.be/dIHbV.
- U.S. Department of Health and Human Services (HHS). Children and Youth Resilience Challenge. https://www.challenge.gov/?challenge=resilience&tab=overview.
- Center for the Study of Social Policy. Youth Thrive: Protective & Promotive Factors for Healthy Development and Well-Being. 2019. https://cssp.org/wp-content/uploads/2019/01/Research-Briefs-and-Action-Sheets-YT-CW.pdf.
- Harvard University Center on the Developing Child. The Science of Resilience. 2015. https://harvardcenter.wpenginepowered.com/wp-content/uploads/2015/05/InBrief-The-Science-of-Resilience.pdf.
- Abrams, Zara. Kids’ Mental Health is In Crisis. Here’s What Psychologists are Doing to Help. American Psychological Association. January 1, 2023. https://www.apa.org/monitor/2023/01/trends-improving-youth-mental-health.
- Haddock, Aaron, et al. Positive Effects of Digital Technology Use by Adolescents: A Scoping Review of the Literature. Int J Environ Res Public Health. 2022 Nov; 19(21): 14009. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9658971/.
- Abi-Jaoude, Elia, Naylor, Karline Treurnict and Pignatiello, Antonio. Smartphones, Social Media Use and Youth Mental Health. CMAJ. 2020 Feb 10; 192(6): E136–E141. doi: 10.1503/cmaj.190434. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7012622/.
- U.S. Surgeon General. Social Media and Youth Mental Health: The U.S. Surgeon General’s Advisory. U.S. Department of Health and Human Services (HHS). 2023. https://www.hhs.gov/sites/default/files/sg-youth-mental-health-social-media-advisory.pdf.
- Weir, Kirsten. Social Media Brings Benefits and Risks to Teens. Psychology Can Help Identify a Path Forward. American Psychological Association. September 1, 2023. https://www.apa.org/monitor/2023/09/protecting-teens-on-social-media.
- Oliver, Meg and Novak, Analisa. Schools Across U.S. Join Growing No-Phone Movement to Boost Focus, Mental Health. CBS News. October 2023. https://www.cbsnews.com/news/schools-no-phone-movement-focus-mental-health/.
- Langreo, Lauraine. Cellphone Bans Can Ease Students’ Stress and Anxiety, Educators Say. Education Week. October 16, 2023. https://www.edweek.org/leadership/cellphone-bans-can-ease-students-stress-and-anxiety-educators-say/2023/10.
- Arundel, Kara. States Ramp Up Efforts to Limit Student Cellphone Use. K-12 Dive. March 11, 2024. https://www.k12dive.com/news/states-limit-student-cell-phone-use-mental-health-learning/709279/.
- Raucoules, Gregory. Cell Phone Use Now Banned at High Schools in Hamblen County. ABC – WATE 6. April 23, 2024. https://www.wate.com/news/hamblen-county-news/most-cell-phone-use-now-banned-at-high-schools/.
- Codispoti, Madi. Local High School Principals Say Proposed Cell Phone Bill is On Par With Current Policies. WJHL – News Channel 11. February 12, 2024. https://www.wjhl.com/news/local/local-high-school-principals-say-proposed-cell-phone-bill-is-on-par-with-current-policies/.
- Lobelville, Tennessee. Perry County District School Cell Phone Policy as of January 17, 2023. 2023. https://lobelvilletn.org/index.php/education/school-cell-phone-policy-as-of-january-17-2023.
- DelPilar, Jackie. Tennessee School District Fines Kids for Using Cell Phones. Is It Legal? Fox 17 – WZTV Nashville. November 30, 2022. https://fox17.com/news/local/a-tn-school-district-fines-kids-for-using-cell-phones-is-it-legal-robertson-county-schools-crisis-in-the-classroom-middle-tennessee-nashville-area-local-news.
- Campbell, Hannah. County Schools To Set District-Wide Policy On Cell Phones At School. Chattanoogan. February 14, 2023. https://www.chattanoogan.com/2023/2/14/464116/County-Schools-To-Set-District-Wide.aspx.
- Shores, Kailee. Why Does MNPS Still Allow Cell Phones in Schools? Nashville Banner. May 22, 2024. https://nashvillebanner.com/2024/05/22/metro-nashville-public-schools-phones-classrooms/.
- Tennessee General Assembly. HB 2758-SB 2809. 2024. https://wapp.capitol.tn.gov/apps/BillInfo/Default.aspx?BillNumber=HB2758.
- Canadian Paediatric Society, Digital Health Task Force. Digital Media: Promoting Healthy Screen Use in School-Aged Children and Adolescents. Paediatr Child Health. 2019 Sep; 24(6): 402–408. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6736327/.
- Darvasi, Paul. How Parents and Educators Can Support Healthy Teen Use of Social Media. October 13, 2021. https://www.kqed.org/mindshift/58624/how-parents-and-educators-can-support-healthy-teen-use-of-social-media.
- Foulkes, Lucy and Andrews, Jack. Are Mental Health Awareness Efforts Contributing to the Rise in Reported Mental Health Problems? A Call to Test the Prevalence Inflation Hypothesis. New Ideas in Psychology, Volume 69, 2023, 101010, ISSN 0732-118X, https://doi.org/10.1016/j.newideapsych.2023.101010. https://www.sciencedirect.com/science/article/pii/S0732118X2300003X.
- Nam, Stella and Urbina-Johanson, Saúl. Navigating Mental Health Literacy, Symptom Beliefs, and Depression Severity: A Commentary on Ahuvia et al., 2023. SSM – Mental Health, Volume 4, 2023, 100282, ISSN 2666-5603, https://doi.org/10.1016/j.ssmmh.2023.100282. https://www.sciencedirect.com/science/article/pii/S266656032300097X.
- Bantjes, Jason, Hunt, Xanthe and Stein, Dan. Anxious, Depressed, and Suicidal: Crisis Narratives in University Student Mental Health and the Need for a Balanced Approach to Student Wellness. Int J Environ Res Public Health. 2023 Mar; 20(6): 4859. doi: 10.3390/ijerph20064859. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10049682/.
- Barry, Ellen. Are We Talking Too Much About Mental Health? New York Times. May 6, 2024. https://www.nytimes.com/2024/05/06/health/mental-health-schools.html.
- Nelson, Kate and England, Adam. These Are the US States Allowing Student Mental Health Days. VeryWell Mind. May 9, 2023. https://www.verywellmind.com/us-states-allowing-student-mental-health-days-5270047.
- Delaware General Assembly. HB 3. 152nd General Assembly. August 16, 2023. https://legis.delaware.gov/BillDetail?LegislationId=130248.
- Ingalls, Nick. Mental Health Days Help Kids, But Systemic Barriers Prevent Widespread Use. Verywell Mind and Parents Magazine. April 27, 2023. https://www.verywellmind.com/mental-health-days-and-kids-survey-6361951.
- National Alliance on Mental Illness (NAMI). NAMI Poll: Parents Want Mental Health Education in Schools, Mental Health Days Off for Students. December 15, 2021. https://www.nami.org/nami-news/nami-poll-parents-want-mental-health-education-in-schools-mental-health-days-off-for-students/.
- Prothero, Arianna. More Schools Are Offering Student Mental Health Days. Here’s What You Need to Know. Education Week. January 19, 2023. https://www.edweek.org/leadership/more-schools-are-offering-student-mental-health-days-heres-what-you-need-to-know/2023/01.
- Gordon, Deb. Best (and Worst) States for Youth Mental Health Care. MoneyGeek. December 20, 2023. https://www.moneygeek.com/insurance/health/analysis/best-states-youth-mental-health/.
- So, Marvin, McCord, Russell F and Kaminski, Jennifer W. Policy Levers to Promote Access to and Utilization of Children’s Mental Health Services: A Systematic Review. Administration and Policy in Mental Health and Mental Health Services Research. 2019. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6531603/.
- Penchansky, R and Thomas, J W. The Concept of Access: Definition and Relationship to Consumer Satisfaction. Medical Care. 1981. https://pubmed.ncbi.nlm.nih.gov/7206846/.
- Kanagaraj, Manoj. Here’s Why Mental Healthcare Is So Unaffordable & How COVID-19 Might Help Change This. Harvard Medical School Center for Primary Care. December 15, 2020. https://info.primarycare.hms.harvard.edu/perspectives/articles/mental-health-unaffordable.
- Pelech, Daria and Hayford, Tamara. Medicare Advantage And Commercial Prices For Mental Health Services. Health Affairs 38, No. 2 (2019): 262–267. https://www.healthaffairs.org/doi/epdf/10.1377/hlthaff.2018.05226.
- U.S. Census Bureau. 2022 American Community Survey 1-Year Estimates. 2023. Available from http://data.census.gov.
- U.S. Treasury, Internal Revenue Service. Requirements Related to the Mental Health Parity and Addiction Equity ACt: A Proposed Rule by the Intenal Revenue Service, the Employee Benefits Security Administration, and the Health and Human Services Department on 08/02/2023. Federal Register: The Daily Journal of the United States Government. August 3, 2023. https://www.federalregister.gov/documents/2023/08/03/2023-15945/requirements-related-to-the-mental-health-parity-and-addiction-equity-act.
- Pestaina, Kaye, et al. Proposed Mental Health Parity Rule Signals Focus on Outcome Data as Tool to Assess Compliance. Kaiser Family Foundation. September 29, 2023. https://www.kff.org/mental-health/issue-brief/proposed-mental-health-parity-rule-signals-new-focus-on-outcome-data-as-tool-to-assess-compliance/.
- Cuello, Leonardo. Final Medicaid Managed Care Rule Explained. Georgetown University Center for Children and Families. May 3, 2024. https://ccf.georgetown.edu/2024/05/03/final-medicaid-managed-care-rule-explained/.
- State of Tennessee. Public Chapter No. 949. May 6, 2024. https://publications.tnsosfiles.com/acts/113/pub/pc0949.pdf.
- Fiscal Review Committee Staff. Corrected Fiscal Memorandum: HB 2921-SB 2801. Tennessee General Assembly. April 9, 2024. https://www.capitol.tn.gov/Bills/113/Fiscal/FM2515.pdf.
- TennCare. Attachment V: Access and Availability for Behavioral Health Services. TennCare Statewide MCO Contract. January 1, 2024. https://www.tn.gov/content/dam/tn/tenncare/documents/MCOStatewideContract.pdf.
- Volk, JoAnn, Goe, Christina and Giovannelli, Justin. Ensuring Access to Behavioral Health Providers. The Commonwealth Fund. January 25, 2024. https://www.commonwealthfund.org/blog/2024/ensuring-access-behavioral-health-providers.
- Hopeful Futures Campaign. State Legislative Guide for School Mental Health. August 2022. https://hopefulfutures.us/wp-content/uploads/2022/09/State-Legislative-Guide-for-School-Mental-Health-1.pdf.
- U.S. Department of Health and Human Services (HHS). Network Adequacy for Behavioral Health: Existing Standards and Considerations for Designing. November 2021. https://aspe.hhs.gov/sites/default/files/documents/792ca3f8d6ae9a8735a40558f53d16a4/behavioral-health-network-adequacy.pdf.
- Pollitz, Karen. Network Adequacy Standards and Enforcement. Kaiser Family Foundation. February 4, 2022. https://www.kff.org/affordable-care-act/issue-brief/network-adequacy-standards-and-enforcement/.
- Melek, Steve, Davenport, Stoddard and Gray, T.J. Addiction and Mental Health vs. Physical Health: Widening Disparities in Network Use and Provider Reimbursement. Milliman. November 19, 2019. https://assets.milliman.com/ektron/Addiction_and_mental_health_vs_physical_health_Widening_disparities_in_network_use_and_provider_reimbursement.pdf.
- McCarthy, Doughlas. The Uses and Benefits of of State APCDs. The Commonwealth Fund. December 2020. https://www.commonwealthfund.org/sites/default/files/2020-12/McCarthy_State_APCDs_Part2_v2.pdf.
- National Academy for State Health Policy. State Definitions of Medical Necessity under the Medicaid EPSDT Benefit. NASHP. April 23, 2021. https://nashp.org/state-tracker/state-definitions-of-medical-necessity-under-the-medicaid-epsdt-bnefit/.
- Burak, Elisabeth Wright. Bipartisan Safer Communities Act Provision Directs CMS to Review State EPSDT Implementation, including in Managed Care. Georgetown University Center for Children and Families. July 27, 2022. https://ccf.georgetown.edu/2022/07/27/bipartisan-safer-communities-act-provision-directs-cms-to-review-state-epsdt-implementation-including-in-managed-care/.
- U.S. Department of Health and Human Services (HHS). New State by State Analysis on Impact of CMS Strategies for States to Protect Children and Youth Medicaid and CHIP Enrollment. December 18, 2023. https://www.hhs.gov/about/news/2023/12/18/new-state-by-state-analysis-on-impact-cms-strategies-for-states-protect-children-youth-medicaid-chip-enrollment.html.
- Georgetown University Center for Children and Families. How Many Children Are Losing Medicaid? May 2024. https://ccf.georgetown.edu/2023/09/27/how-many-children-are-losing-medicaid/.
- Artiga, Samantha, Rudowitz, Robin and Tolbert, Jennifer. Outreach and Enrollment Strategies for Reaching the Medicaid Eligible but Uninsured Population . Kaiser Family Foundation. March 2, 2016. https://www.kff.org/medicaid/issue-brief/outreach-and-enrollment-strategies-for-reaching-the-medicaid-eligible-but-uninsured-population/.
- Wachino, Victoria and Weiss, Alice. Maximizing Kids’ Enrollment in Medicaid and SCHIP: What Works in Reaching, Enrolling and Retaining Eligible Children. National Academy for State Health Policy and Robert Wood Johnson Foundation. February 2009. https://ccf.georgetown.edu/wp-content/uploads/2012/03/maximizing-kids-enrollment.pdf.
- Healthy Students, Promising Futures. Map: School Medicaid Programs. Healthy Students, Promising Futures. June 2021. https://healthystudentspromisingfutures.org/map-school-medicaid-programs/.
- National Association of Social Workers. NASW Standards for School Social Work Services. 2012. https://www.socialworkers.org/Practice/NASW-Practice-Standards-Guidelines/NASW-Standards-for-School-Social-Work-Services.
- National Association of School Psychologists. State Shortages Data Dashboard. February 2024. https://www.nasponline.org/about-school-psychology/state-shortages-data-dashboard.
- Tennessee Department of Education (TDOE). 2023 Annual Statistical Report. May 2024. https://www.tn.gov/education/districts/federal-programs-and-oversight/data/department-reports/2023-annual-statistical-report.html.
- Hopeful Futures. America’s School Mental Health Report Card. February 2022. https://hopefulfutures.us/wp-content/uploads/2022/02/Final_Master_021522.pdf.
- Mental Health America. Addressing The Youth Mental Health Crisis: The Urgent Need For More Education, Services, And Supports. July 2021. https://mhanational.org/sites/default/files/FINAL%20MHA%20Report%20-%20Addressing%20Youth%20Mental%20Health%20Crisis%20-%20July%202021.pdf.
- Rivera, Autumn. To Address Student Well-Being, States Increase Access to Mental Health in Schools. National Conference of State Legislatures. May 24, 2023. https://www.ncsl.org/state-legislatures-news/details/to-address-student-well-being-states-increase-access-to-mental-health-in-schools.
- State of Tennessee. Public Chapter No. 910. May 3, 2024. https://publications.tnsosfiles.com/acts/113/pub/pc0910.pdf.
- California Department of Health Care Access and Information. California Introduces New Wellness Coach Program Aimed at Building a More Diverse Behavioral Health Workforce to Help Children and Youth. December 21, 2023. https://hcai.ca.gov/california-introduces-new-wellness-coach-program-aimed-at-building-a-more-diverse-behavioral-health-workforce-to-help-children-and-youth/.
- State of California. Broad Behavioral Health Workforce Capacity. Child and Youth Behavioral Health Initiative. 2024. https://cybhi.chhs.ca.gov/workstream/broad-behavioral-health-workforce-capacity/.
- Figaro, Wildaline, McCann, Jessica and Juarez, Tonantzin. Community Health Workers Can Help Improve Youth Mental Health. Health Affairs. May 10, 2024. https://www.healthaffairs.org/content/forefront/community-health-workers-can-help-improve-youth-mental-health.
- State of California. Youth Peer-to-Peer Support Program. Child and Youth Behavioral Health Initiative. 2024. https://cybhi.chhs.ca.gov/workstream/youth-peer-to-peer-support-program/.
- Tennessee Department of Mental Health and Substance Abuse Services (TDMHSAS). Certified Young Adult Peer Support Specialist. https://www.tn.gov/behavioral-health/mental-health-services/peers/cyapss.html.
- Abramson, Ashley. Children’s Mental Health Is In Crisis. American Psychological Association. January 1, 2022. https://www.apa.org/monitor/2022/01/special-childrens-mental-health.
- Tennessee Department of Mental Health and Substance Abuse Services (TDMHSAS). Faith-Based Initiatives. https://www.tn.gov/behavioral-health/faith.html.
- Tyler, Elizabeth Tobin, Hulkower, Rachel and Kaminski, Jennifer. Behavioral Health Integration in Pediatric Primary Care: Considerations and Opportunities for Policymakers, Planners, and Providers. Milbank Memorial Fund. March 15, 2017. https://www.milbank.org/publications/behavioral-health-integration-in-pediatric-primary-care-considerations-and-opportunities-for-policymakers-planners-and-providers/.
- U.S. Department of Health and Human Services (HHS). Joint Dear Colleague Letter on Children’s Mental Health. May 25, 2022. https://www.hrsa.gov/sites/default/files/hrsa/about/news/2022-joint-letter-childrens-mental-health.pdf.
- BRAIN Center Memphis. Home. https://braincentermemphis.org/.
- Bipartisan Policy Center. Tackling America’s Mental Health and Addiction Crisis Through Primary Care Integration. March 2021. https://bipartisanpolicy.org/download/?file=/wp-content/uploads/2021/03/BPC_Behavioral-Health-Integration-report_R03.pdf.
- Information provided. Data provided to the Sycamore Institute by the Tennessee Commission on Children & Youth on July 26, 2023.
- Panchal, Nirmita, Cox, Cynthia and Rudowitz, Robin. The Landscape of School-Based Mental Health Services. Kaiser Family Foundation. September 6, 2022. https://www.kff.org/mental-health/issue-brief/the-landscape-of-school-based-mental-health-services/.
- Division of TennCare. TennCare School-Based Services Presentation. December 2023.
- State of California. Statewide Multi-Payer Fee Schedule for School-Linked Behavioral Health Services. Children and Youth Behavioral Health Initiative. 2024. https://cybhi.chhs.ca.gov/workstream/statewide-multi-payer-fee-schedule-for-school-linked-behavioral-health-services/.
- U.S. Centers for Disease Control and Prevention (CDC). Public Health Strategies for Rural Child Mental Health: Policy Brief. May 15, 2024. https://www.cdc.gov/rural-health/php/public-health-strategy/strategies-for-child-health-policy-brief.html

