Access to affordable, healthy food is a driver of health and well-being. Food insecurity occurs when a household has limited access to food. (1) Households that experience food insecurity have an increased risk of negative health outcomes such as cardiovascular disease and diabetes.
Research shows that food insecure adults are also more likely to be obese than food secure adults. (2) The correlation between food insecurity and obesity may seem counterintuitive, but they actually share many of the same risk factors.
What is Food Insecurity?
According to the U.S. Department of Agriculture (USDA) data, households considered food secure “have consistent, dependable access to enough food for active, healthy living.” Food insecurity, on the other hand, occurs when households have limited or uncertain access to nutritious foods because of money or other resource constraints. (1) (3)
- Food insecure households spend 27% less on food compared to food secure households.(1)
- When households experience food insecurity, they are typically food insecure for 7 months out of the year.(1)
Figure 1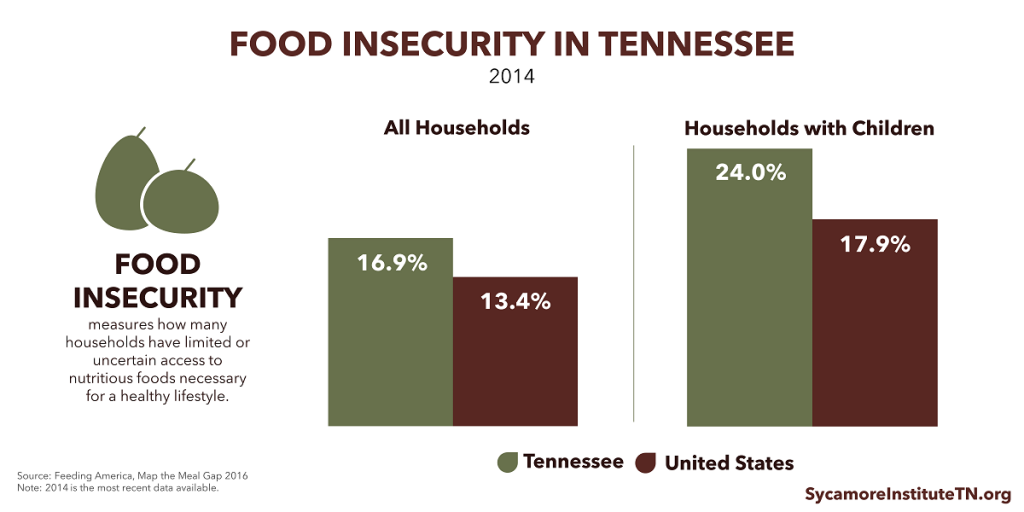
Food Insecurity in Tennessee
- 17% of households in Tennessee are food insecure. (Figure 1)
- Tennessee is one of 12 states with a food insecurity rate higher than the national average by a statistically significant amount.(1)
- The prevalence of food insecurity varies greatly across the state – from 8% of all households in Williamson County to 23% in Haywood County.(3) (Figure 2)
- Food insecurity rates among households with children range from 15% in Williamson County to 32% in Cocke County.(3) (Figure 3)
Figure 2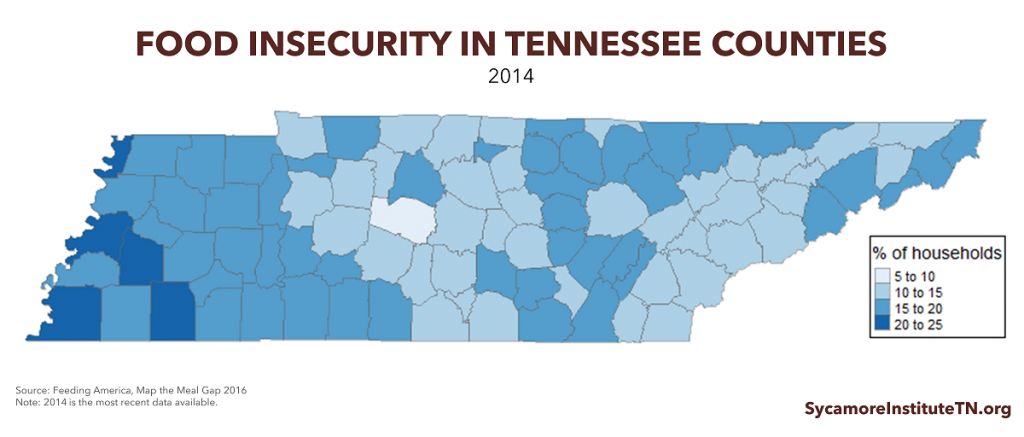
Adverse Consequences of Food Insecurity
Food insecurity is associated with a variety of negative outcomes, including: (4)
- A higher rate of diabetes, obesity, and cardiovascular disease,
- Decreased school performance and cognitive development among children,
- Iron deficiency anemia and increased risk of hospitalization among children,
- Decreased worker productivity due to related health conditions, and
- Poor maternal nutrition, which is important for fetal development and a healthy pregnancy.
Figure 3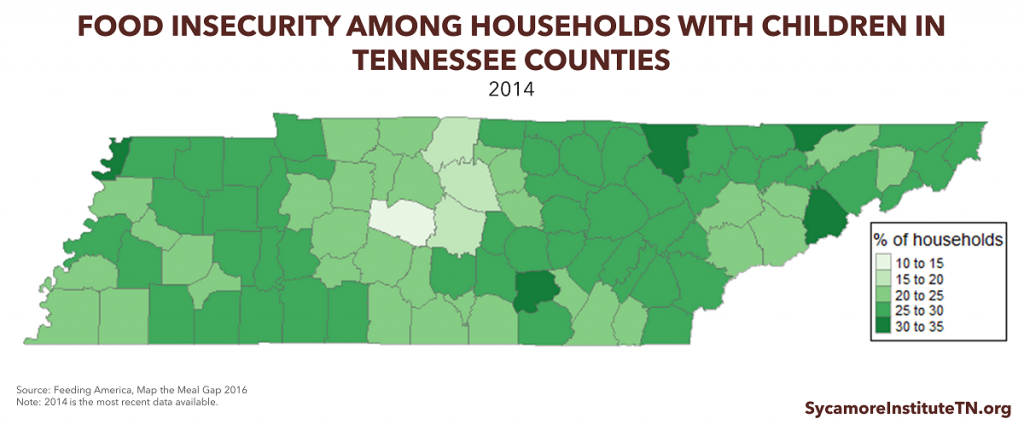
What Is Obesity?
Obesity is defined as having a Body Mass Index (BMI) of 30.0 or higher. (5) Non-Hispanic Blacks, Hispanics, older and middle aged adults, and low-income women are more likely to be obese compared to other groups. (6)
Obesity in Tennessee
- Tennessee has a higher obesity rate than the United States average (Figure 4). Similar to Tennessee, other southern states have higher obesity rates than other parts of the United States.(7)
- Adult obesity rates vary greatly across the state – Williamson County had the lowest rate (26%), and McNairy County had the highest rate (39%) (Figure 5).
- Measures of obesity do not include individuals who are considered overweight, which is defined as having a BMI between 25.0 and 29.9. 69% of Tennessee adults are considered overweight or obese, compared to 65% nationally. (8)
Figure 4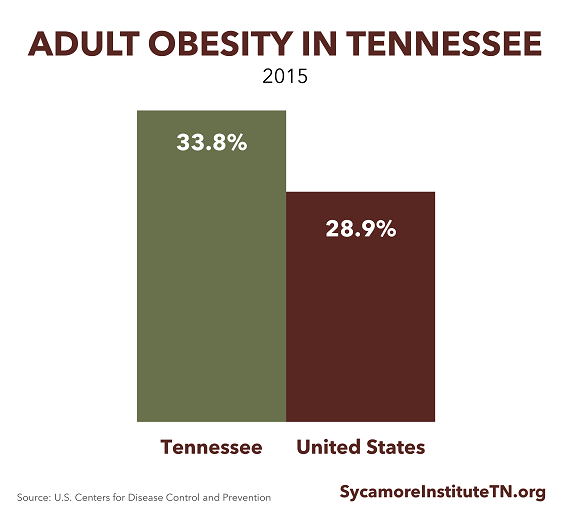
Figure 5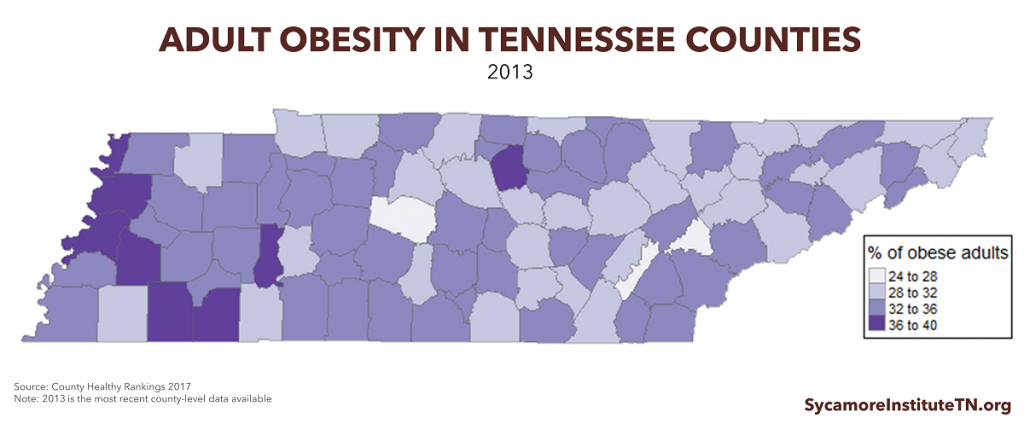
Food Insecurity and Obesity in Tennessee
Food insecure adults in Tennessee and nationwide are more likely to be obese than food secure adults. The rates of food insecurity and obesity in Tennessee counties show positive correlation. This means that as one increases or decreases, so does the other (Figure 6). (9)
Research also shows that the food insecurity-obesity link is strongest among women nationally. (10) Food insecure children may also be more likely to be overweight, but the evidence is mixed. (10) (11)
Figure 6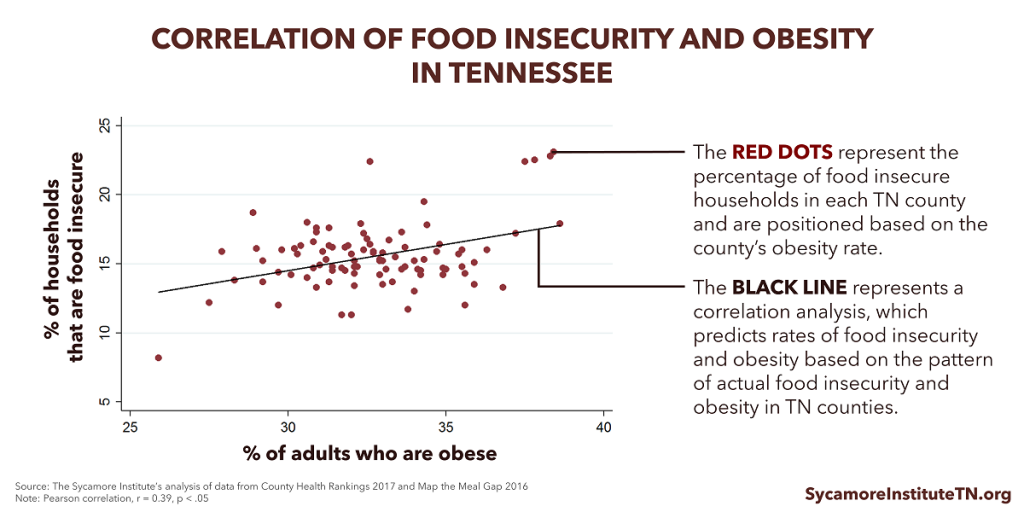
What Factors Link Food Insecurity and Obesity?
Food insecurity does not cause obesity, but research shows an association between the two. Food insecurity and obesity often exist in the same environments because both are linked to many of the same risk factors and social and economic challenges. (12)
A mix of individual behaviors and characteristics, household factors, and social and economic environments influence food insecurity and obesity. These factors are often complex and interconnected. (4) For example, the following types of households are more likely to experience higher rates of food insecurity both in Tennessee and the U.S.:
- Low-income households,
- African American, American Indian, and Hispanic households,
- Households with children, and
- Households that include someone with a disability. (4)
Economic and environmental factors like food and energy prices, housing costs, and unemployment rates also influence food insecurity rates. (4) (See our report The Housing and Health Connection.)
The risk factors for obesity are also complex and include individual health behaviors and environmental factors. Unhealthy eating patterns and a lack of physical activity can both contribute to obesity. Environmental factors also influence risks for obesity — including access to healthy and affordable food, neighborhood exposure to fast food restaurants, access to recreational facilities and parks, and the comparative costs of foods with greater nutritional value and fewer calories. (13) (14)
How the Risk Factors Overlap
The risk factors outlined above overlap in ways in that contribute to both food insecurity and obesity.
Food insecurity may lead to a cycle of food deprivation and overeating, which can cause obesity. When food is scarce, people facing food insecurity may miss meals or eat less. When food is abundant, people dealing with food insecurity tend to binge and overeat. This type of eating pattern is associated with increased body fat and weight gain. (15)
The resources available in a neighborhood can contribute to both food insecurity and obesity. For example, low-income communities are less likely to have a full-service grocery store or farmers market that sell nutritious foods. On the other hand, these communities often have fast-food restaurants and neighborhood corner stores that sell foods with less nutritional value.
Income contributes to food security while influencing the choices that affect obesity. Having a low-income is the greatest risk factor for food insecurity. (4) Income determines the ability to buy and access needed services. When resources are limited, households must choose between housing, transportation, health care, food costs, and other needs. To make ends meet, households may buy less expensive, high-calorie, and energy-dense foods instead of more costly, higher quality foods. (12)
Access to transportation can influence both food insecurity and obesity. “Vehicle access is perhaps the most important determinant of whether or not a family can access affordable nutritious food,” according to USDA. (16) If families cannot get nutritious food in their own neighborhoods, their access to it depends on having reliable transportation. At the same time, transportation and infrastructure systems affect the types of opportunities and amount of time people have to engage in physical activities that help maintain a healthy weight. (See our report How Transportation Impacts Public Health.)
Food insecurity contributes to stress and poor mental health, which is a risk factor for weight gain. The financial pressures of food insecurity, living in a resource-poor neighborhood, and lack of access to other needed services are associated with poor mental health, stress, and weight gain. Weight gain often results from stress-induced hormonal changes, poor eating habits, and physical inactivity. (12)
More Information About the Drivers of Health
To learn more about the factors that influence health and well-being in across our state, check out The Drivers of Health: 4 Factors that Influence Individual and Population Health.
References
Click to Open/Close
1. Coleman-Jensen, Alisha, et al. Household Food Security in the United States. U.S. Department of Agriculture, Economic Research Service, September 2016. [Online] September 2016. https://www.ers.usda.gov/webdocs/publications/err215/err-215.pdf?v=42636.
2. Martin, Katie S and Ferris, Ann M. Food Insecurity and Gender are Risk Factors for Obesity. Journal of Nutrition Education and Behavior, 39(1). [Online] 2007. http://s3.amazonaws.com/academia.edu.documents/41249175/Food_insecurity_and_gender_are_risk_fact20160115-8784-ud662j.pdf?AWSAccessKeyId=AKIAIWOWYYGZ2Y53UL3A&Expires=1492793377&Signature=AbNhFTHVfAlBT34ZhmXXrugGwnU%3D&response-content-disposition=inline%3B.
3. Feeding America. Map the Meal Gap 2016: Highlights of Findings for Overall and Child Food Insecurity. Map the Meal Gap. [Online] http://www.feedingamerica.org/hunger-in-america/our-research/map-the-meal-gap/2014/map-the-meal-gap-2014-exec-summ.pdf.
4. RTI International, Center for Health and Environmental Modeling. Current and Propsective Scope of Hunger and Food Security in America: A Review of Current Research. [Online] July 2014. http://www.rti.org/sites/default/files/resources/full_hunger_report_final_07-24-14.pdf.
5. Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion. Defining Adult Overweight and Obesity. Centers for Disease Control and Prevention. [Online] 2016. https://www.cdc.gov/obesity/adult/defining.html.
6. —. Adult Obesity Facts. Centers for Disease Control. [Online] 2016. https://www.cdc.gov/obesity/data/adult.html.
7. —. Adult Obesity Prevalence Maps. Centers for Disease Control. [Online] 2017. https://www.cdc.gov/obesity/data/prevalence-maps.html
8. National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. BRFSS Prevalence & Trends Data 2015. Center for Disease Control and Prevention. [Online] https://www.cdc.gov/brfss/brfssprevalence/.
9. The Sycamore Institute. Sycamore Institute analysis of County Health Rankings 2017 data and Map the Meal Gap 2016 data. [Online] 2017.
10. Franklin, Brandi, et al. Exploring Mediators of Food Insecurity and Obesity: A Review of Recent Literature. Journal of Community Health, 37(1), 253-264. [Online] 2012. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3334290/pdf/nihms365575.pdf.
11. Casey, Patrick H, et al. The Association of Child and Household Food Insecurity with Childhood Overweight Status. Pediatrics. [Online] 2006. https://pediatrics.aappublications.org/content/118/5/e1406
12. Food Research & Action Center. Understanding the Connections: Food Insecurity and Obesity. Food Research & Action Center. [Online] October 2015. http://frac.org/wp-content/uploads/frac_brief_understanding_the_connections.pdf.
13. Faith, Myles S and Kral, Tanja VE. Social environmental and genetic influences on obesity and obesity-promoting behaviors: Fostering research integration. Genes, Behavior, and the Social Environment: Moving Beyond the Nature/Nurture Debate. [Online] 2006. https://www.ncbi.nlm.nih.gov/books/NBK19935/.
14. The Centers for Disease Control and Prevention. Adult Obesity Causes & Consequences. Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion. [Online] August 2016. https://www.cdc.gov/obesity/adult/causes.html.
15. Dinour, Lauren M, Bergen, Dara and Yeh, Ming-Chin. The Food Insecurity-Obesity Paradox: A Review of the Literature and the Role Food Stamps May Play. Journal of the American Dietetic Association. [Online] 2007. http://www.andjrnl.org/article/S0002-8223(07)01616-1/pdf.
16. United States Department of Agriculture. Access to Affordable and Nutritious Food: Measuring and Understanding Food Deserts and Their Consequences. Economic Research Service, United States Department of Agriculture. [Online] June 2009. https://www.ers.usda.gov/webdocs/publications/42711/12698_ap036fm_1_.pdf?v=0
17. Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion. Adult Obesity Causes & Consequences. Centers for Disease Control. [Online] 2016. https://www.cdc.gov/obesity/adult/causes.html.

